Us Rx Care Pa Form
Us Rx Care Pa Form - Our team is able to review and respond to most prior authorization requests within 24 hours if not the same day. Incomplete forms may delay processing. Quality of care and service obsessed. Contractual adherence to fiduciary standards on behalf of plan sponsors and plan enrollees. For prior authorization requests simply complete our short pa form and fax to us. There may be a drug specific fax form available** provider information member information prescriber name (print) member name (print) Web request for prior authorization (pa) must include the member name, id#, dob, and drug name. Incomplete forms may delay processing. Sign it in a few clicks draw your signature, type it, upload its image, or use your mobile device as a signature pad. Incomplete forms will delay processing.
Incomplete forms will delay processing. Our team is able to review and respond to most prior authorization requests within 24 hours if not the same day. Quality of care and service obsessed. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Our team is able to review and respond to most prior authorization requests within 24. Request for prior authorization (pa) must include member name, id#, dob and drug name. Sign it in a few clicks draw your signature, type it, upload its image, or use your mobile device as a signature pad. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Edit your us rx care prior authorization form online type text, add images, blackout confidential details, add comments, highlights and more. Web request for prior authorization (pa) must include the member name, id#, dob, and drug name.
There may be a drug specific fax form available** provider information member information prescriber name (print) member name (print) Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Incomplete forms may delay processing. Request for prior authorization (pa) must include member name, id#, dob and drug name. Web reimbursement form if you are a member filing a paper claim for medication (s) purchased, please complete the direct member reimbursement form and fax it to the number. Web us rx care will respond via fax or phone within 24 hours of all necessary information, except during weekends and holidays. Our team is able to review and respond to most prior authorization requests within 24 hours if not the same day. For prior authorization requests simply complete our short pa form and fax to us. Sign it in a few clicks draw your signature, type it, upload its image, or use your mobile device as a signature pad. Web request for prior authorization (pa) must include the member name, id#, dob, and drug name.
RightMed Save on your medications today!
Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Request for prior authorization (pa) must include member name, id#, dob and drug name. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). For prior authorization requests simply complete our short pa form and fax to us. Incomplete forms.
USRx Care Fiduciary Pharmacy Benefit Services YouTube
Incomplete forms may delay processing. Web us rx care will respond via fax or phone within 24 hours of all necessary information, except during weekends and holidays. Request for prior authorization (pa) must include member name, id#, dob and drug name. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Sign it.
Home
For prior authorization requests simply complete our short pa form and fax to us. Incomplete forms may delay processing. Contractual adherence to fiduciary standards on behalf of plan sponsors and plan enrollees. Web reimbursement form if you are a member filing a paper claim for medication (s) purchased, please complete the direct member reimbursement form and fax it to the.
Optum Rx Pa Form Fill and Sign Printable Template Online US Legal Forms
Web us rx care will respond via fax or phone within 24 hours of all necessary information, except during weekends and holidays. Web reimbursement form if you are a member filing a paper claim for medication (s) purchased, please complete the direct member reimbursement form and fax it to the number. Request for prior authorization (pa) must include member name,.
USRx Care
Web request for prior authorization (pa) must include the member name, insurance, id#, date of birth, and drug name. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Quality of care and service obsessed. Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: For prior authorization requests simply.
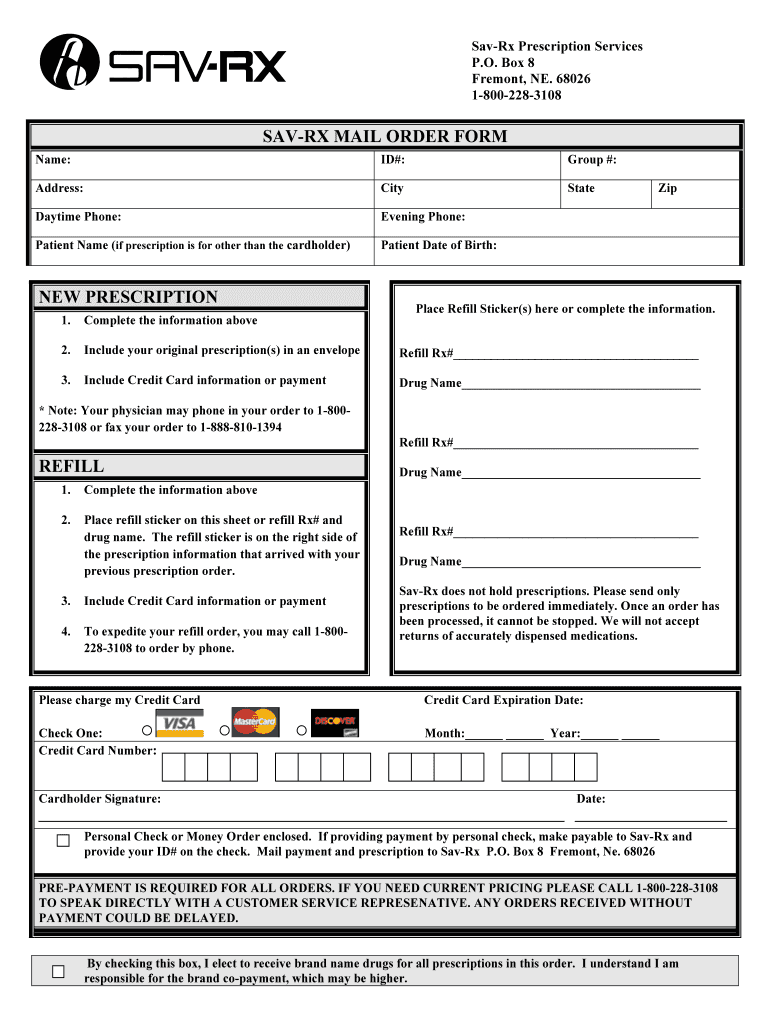
Savrx Pa Form Fill Out and Sign Printable PDF Template signNow
Request for prior authorization (pa) must include member name, id#, dob and drug name. Quality of care and service obsessed. Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Incomplete forms may delay processing. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.).
quest requisition form fill online printable fillable blank pdffiller
Quality of care and service obsessed. Incomplete forms may delay processing. For prior authorization requests simply complete our short pa form and fax to us. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Sign it in a few clicks draw your signature, type it, upload its image, or use your mobile.
A request for prior authorization has been denied for lack of information received from the prescriber. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Share your form with others Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: There may be a drug specific fax form available**.
Reviews Pharmacy That Lacks Feedback RxStars RxStars
Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Web request for prior authorization (pa) must include the member name, id#, dob, and drug name. Web reimbursement form if you are a member filing a paper claim for medication (s) purchased, please complete the direct member reimbursement form and fax it to the number. Our team.
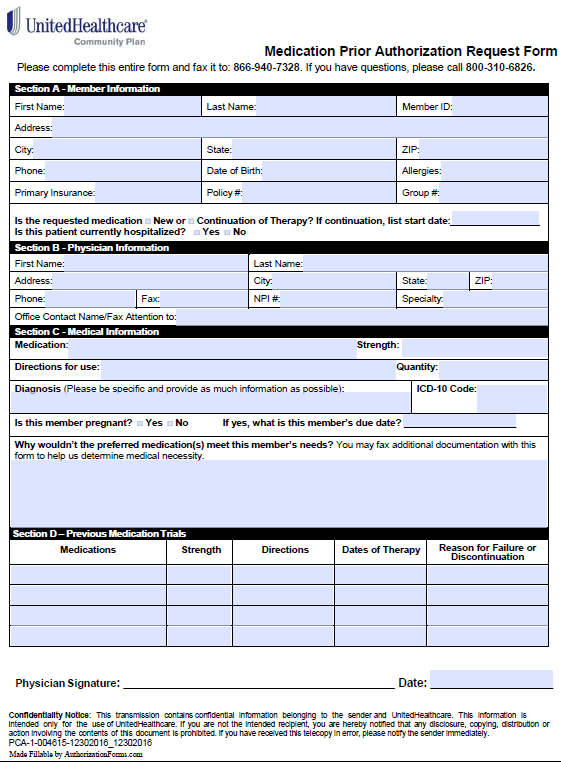
Free United Healthcare Prior Prescription (Rx) Authorization Form PDF
Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Web request for prior authorization (pa) must include the member name, id#, dob, and drug name. Our team is able to review and respond to most prior authorization requests within 24. Web request for prior authorization (pa) must include the member name, insurance, id#, date of birth,.
Share Your Form With Others
There may be a drug specific fax form available** provider information member information prescriber name (print) member name (print) Incomplete forms may delay processing. Edit your us rx care prior authorization form online type text, add images, blackout confidential details, add comments, highlights and more. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.).
For Prior Authorization Requests Simply Complete Our Short Pa Form And Fax To Us.
Incomplete forms will delay processing. Web medication prior authorization form **please fax request to 888‐389‐9668 or mail to: Our team is able to review and respond to most prior authorization requests within 24. Web request for prior authorization (pa) must include the member name, id#, dob, and drug name.
Web Us Rx Care Will Respond Via Fax Or Phone Within 24 Hours Of All Necessary Information, Except During Weekends And Holidays.
A request for prior authorization has been denied for lack of information received from the prescriber. Please include lab reports with request when appropriate (e.g., c&s, hga1c, serum cr, cd4, h&h, wbc, etc.). Sign it in a few clicks draw your signature, type it, upload its image, or use your mobile device as a signature pad. Incomplete forms may delay processing.
Web Reimbursement Form If You Are A Member Filing A Paper Claim For Medication (S) Purchased, Please Complete The Direct Member Reimbursement Form And Fax It To The Number.
Web request for prior authorization (pa) must include the member name, insurance, id#, date of birth, and drug name. Request for prior authorization (pa) must include member name, id#, dob and drug name. Contractual adherence to fiduciary standards on behalf of plan sponsors and plan enrollees. Our team is able to review and respond to most prior authorization requests within 24 hours if not the same day.