Tufts Prior Authorization Form
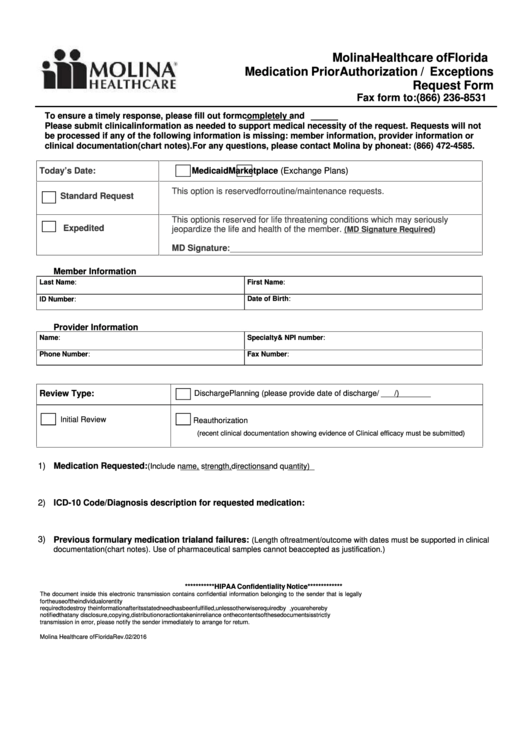
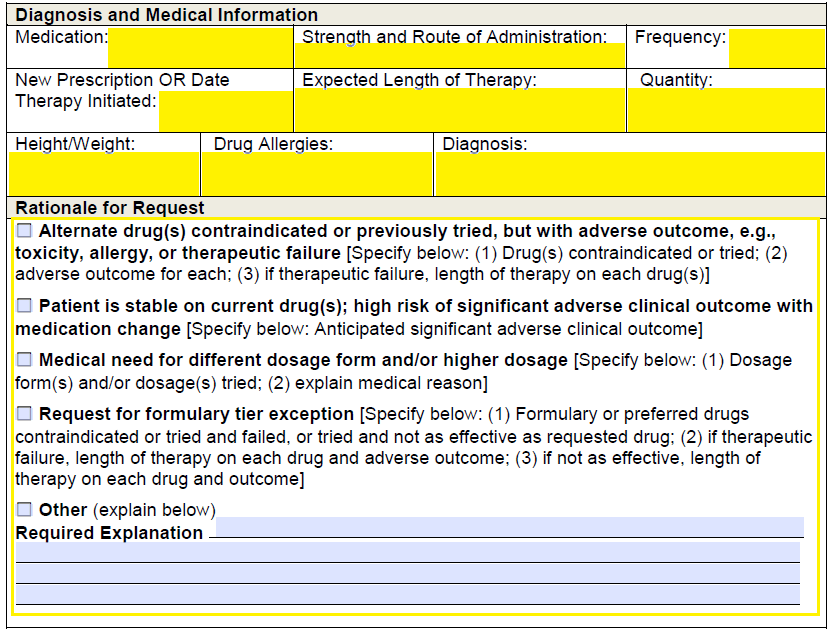
Tufts Prior Authorization Form - For payer specific policies, please reference the payer specific websites. The paf must be completed and submitted to the insurance company before any treatment or procedure can be performed. Web prior authorizations a prior authorization (pa) may be required to determine medical necessity and appropriateness of certain health care services. This means that you will need to get approval from tufts medicare preferred hmo before you fill your prescriptions. You may need to renew your coverage this year. Services that may require prior authorization include surgical services, durable medical equipment (dme), and/or prescription drugs. Please fax the completed form to the plan listed below: Web the tufts prior authorization form, also known as the paf, is a document that medical professionals use to request authorization from insurance companies for specific treatments or procedures. Web view form called 2023 tufts health plan medicare preferred pre enrollment checklist. For prior authorization (pa) information for medical services, refer to the following:
Web the tufts prior authorization form, also known as the paf, is a document that medical professionals use to request authorization from insurance companies for specific treatments or procedures. Providers may attach any additional clinical data or documentation relevant to this request. Web this form is for physicians to submit information to tufts health plan to help determine drug coverage for tufts health plan medicare preferred, tufts health plan senior care options, tufts health unify and proper payment under medicare part b versus part d per the centers for medicare and medicaid services (cms). 2023 tufts medicare preferred individual enrollment form. For prior authorization (pa) information for medical services, refer to the following: For pa information for behavioral health services, refer to the following: Please note, this form is intended for new enrollments. Tufts medicare preferred hmo requires you or your physician to get prior authorization for certain drugs. You may need to renew your coverage this year. Referral, prior authorization and notification policy.
This form is used to apply for enrollment in a tufts health plan medicare preferred plans. Tufts health public plans provider manual. Referral, prior authorization and notification policy. Providers should consult the health plan’s coverage policies, member benefits, and medical necessity guidelines to complete this form. For pa information for behavioral health services, refer to the following: Tufts medicare preferred hmo requires you or your physician to get prior authorization for certain drugs. For prior authorization (pa) information for medical services, refer to the following: Web tufts health plan medication prior authorization request form. Providers may attach any additional clinical data or documentation relevant to this request. • tufts health plan commercial plans;
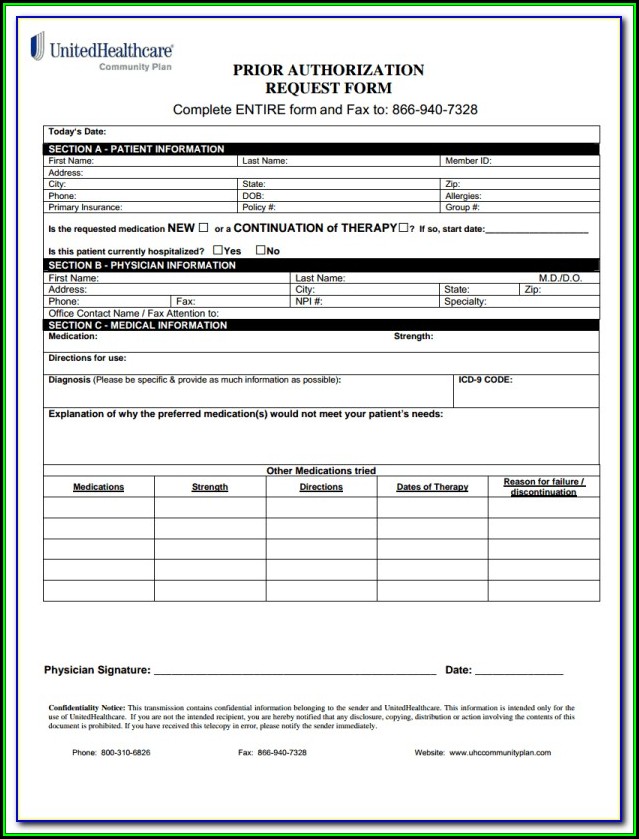
Aarp Prior Authorization Form Form Resume Examples dP9lDOk9RD
Tufts health public plans provider manual. Referral, prior authorization and notification policy. Web the tufts prior authorization form, also known as the paf, is a document that medical professionals use to request authorization from insurance companies for specific treatments or procedures. Tufts medicare preferred hmo requires you or your physician to get prior authorization for certain drugs. Web prior authorizations.
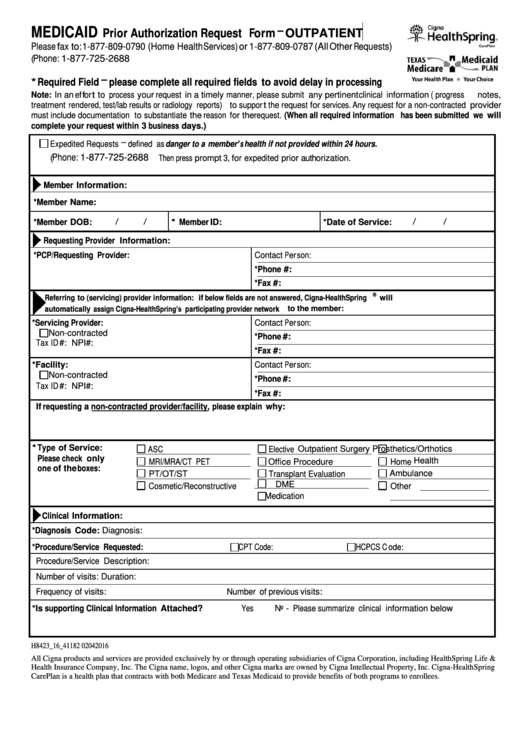
Fillable Medicaid Prior Authorization Request Form Outpatient Cigna
This form is used to apply for enrollment in a tufts health plan medicare preferred plans. Referral, prior authorization and notification policy. This means that you will need to get approval from tufts medicare preferred hmo before you fill your prescriptions. The paf must be completed and submitted to the insurance company before any treatment or procedure can be performed..
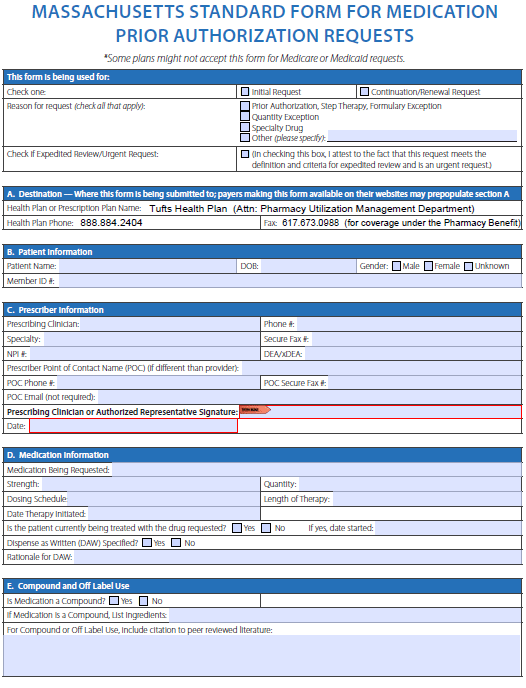
Free TUFTS Prior Prescription (Rx) Authorization Form PDF
This form is used to apply for enrollment in a tufts health plan medicare preferred plans. 2023 tufts medicare preferred individual enrollment form. Services that may require prior authorization include surgical services, durable medical equipment (dme), and/or prescription drugs. Web standardized prior authorization request form reference guide the standardized prior authorization request form is not intended to replace payer specific.
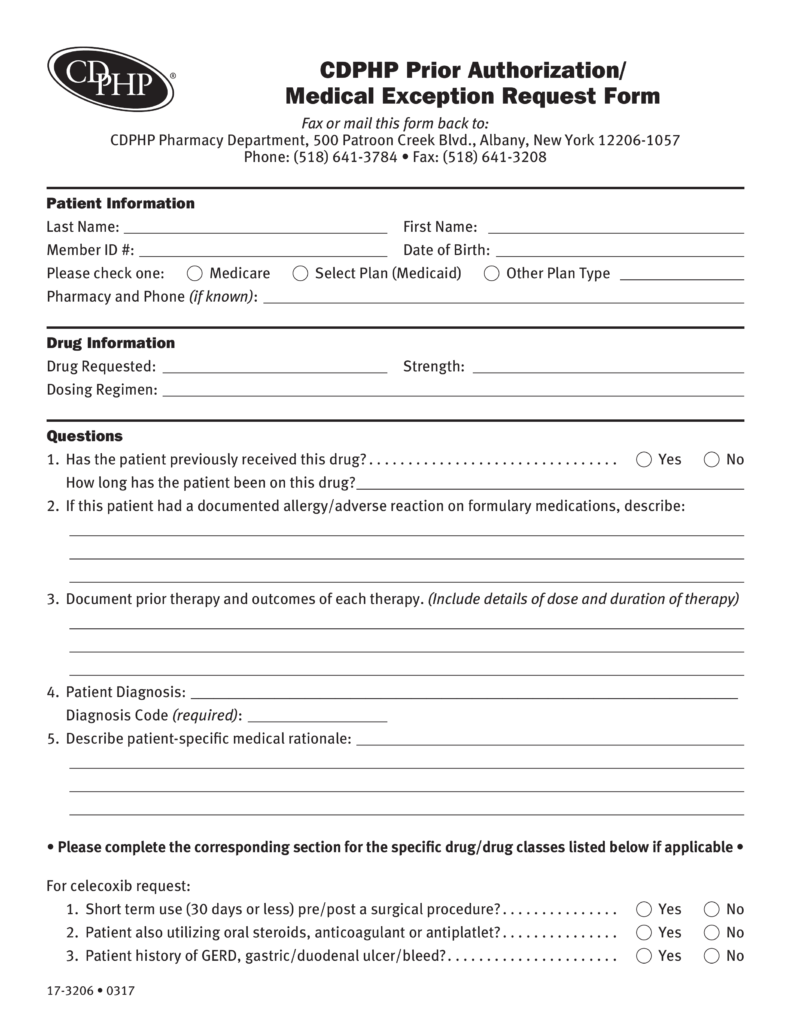
Free CDPHP Prior (Rx) Authorization Form PDF eForms
Please fax the completed form to the plan listed below: You may need to renew your coverage this year. For prior authorization (pa) information for medical services, refer to the following: Referral, prior authorization and notification policy. Tufts health public plans provider manual.
22 Medicare Prior Authorization Form Templates Free To Download In PDF
Tufts health public plans provider manual. Please fax the completed form to the plan listed below: For prior authorization (pa) information for medical services, refer to the following: For pa information for behavioral health services, refer to the following: Web view form called 2023 tufts health plan medicare preferred pre enrollment checklist.
Tufts Prior Auth form Elegant Cardiovascular Drug Development
For payer specific policies, please reference the payer specific websites. This form is used to apply for enrollment in a tufts health plan medicare preferred plans. Please note, this form is intended for new enrollments. Web this form is for physicians to submit information to tufts health plan to help determine drug coverage for tufts health plan medicare preferred, tufts.
Tufts Medicare Prior Authorization form Fresh Medical
Web the tufts prior authorization form, also known as the paf, is a document that medical professionals use to request authorization from insurance companies for specific treatments or procedures. • tufts health plan commercial plans; For prior authorization (pa) information for medical services, refer to the following: Providers should consult the health plan’s coverage policies, member benefits, and medical necessity.
25 Medicare Prior Authorization Form Templates free to download in PDF
Please note, this form is intended for new enrollments. For payer specific policies, please reference the payer specific websites. Providers should consult the health plan’s coverage policies, member benefits, and medical necessity guidelines to complete this form. Web tufts health plan medication prior authorization request form. You may need to renew your coverage this year.
Tufts Prior Auth form Elegant the Willcutts Report
Providers should consult the health plan’s coverage policies, member benefits, and medical necessity guidelines to complete this form. Web standardized prior authorization request form reference guide the standardized prior authorization request form is not intended to replace payer specific prior authorization procedures, policies and documentation requirements. Referral, prior authorization and notification policy. Web prior authorizations a prior authorization (pa) may.
Free Wellcare Prior Prescription (Rx) Authorization Form PDF
• tufts health plan commercial plans; For pa information for behavioral health services, refer to the following: Providers should consult the health plan’s coverage policies, member benefits, and medical necessity guidelines to complete this form. Providers may attach any additional clinical data or documentation relevant to this request. Tufts medicare preferred hmo requires you or your physician to get prior.
2023 Tufts Medicare Preferred Individual Enrollment Form.
Web tufts health plan medication prior authorization request form. Referral, prior authorization and notification policy. Please fax the completed form to the plan listed below: • tufts health plan commercial plans;
Web The Tufts Prior Authorization Form, Also Known As The Paf, Is A Document That Medical Professionals Use To Request Authorization From Insurance Companies For Specific Treatments Or Procedures.
Please note, this form is intended for new enrollments. Tufts health public plans provider manual. Web standardized prior authorization request form reference guide the standardized prior authorization request form is not intended to replace payer specific prior authorization procedures, policies and documentation requirements. For payer specific policies, please reference the payer specific websites.
You May Need To Renew Your Coverage This Year.
Providers should consult the health plan’s coverage policies, member benefits, and medical necessity guidelines to complete this form. Web prior authorizations a prior authorization (pa) may be required to determine medical necessity and appropriateness of certain health care services. This means that you will need to get approval from tufts medicare preferred hmo before you fill your prescriptions. Providers may attach any additional clinical data or documentation relevant to this request.
The Paf Must Be Completed And Submitted To The Insurance Company Before Any Treatment Or Procedure Can Be Performed.
For pa information for behavioral health services, refer to the following: This form is used to apply for enrollment in a tufts health plan medicare preferred plans. Services that may require prior authorization include surgical services, durable medical equipment (dme), and/or prescription drugs. For prior authorization (pa) information for medical services, refer to the following: