Request For Authorization Form
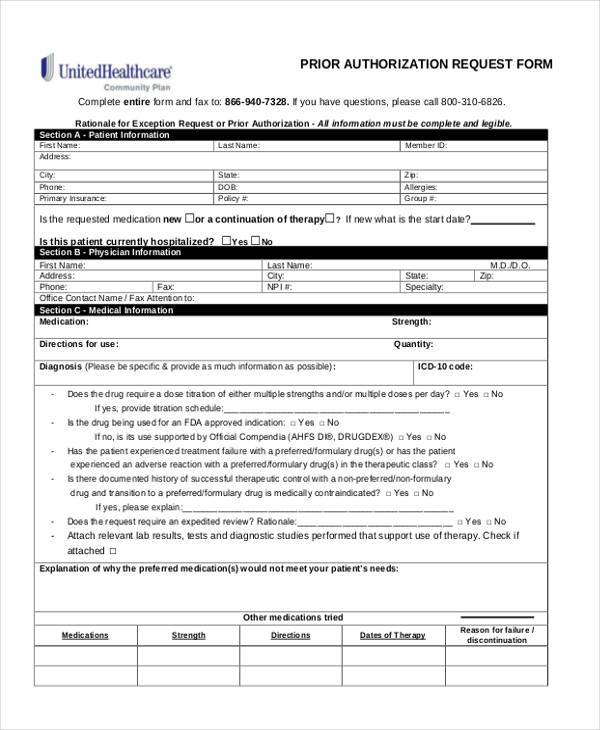
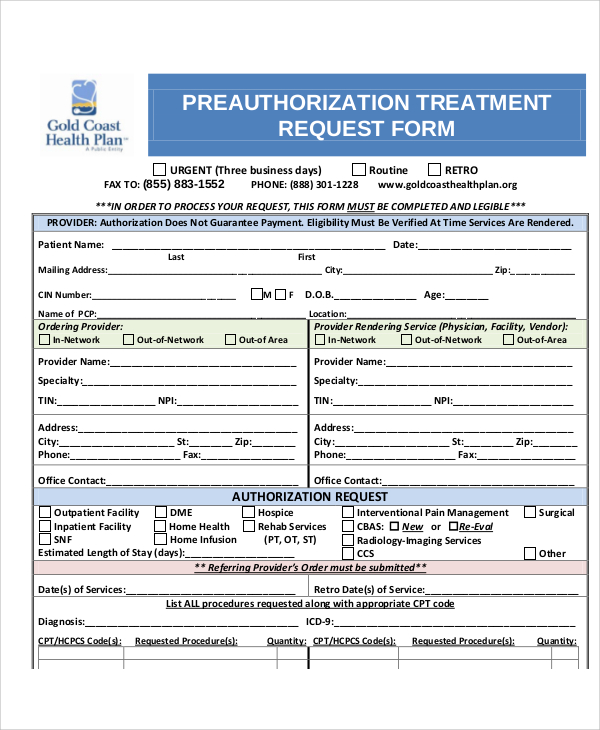
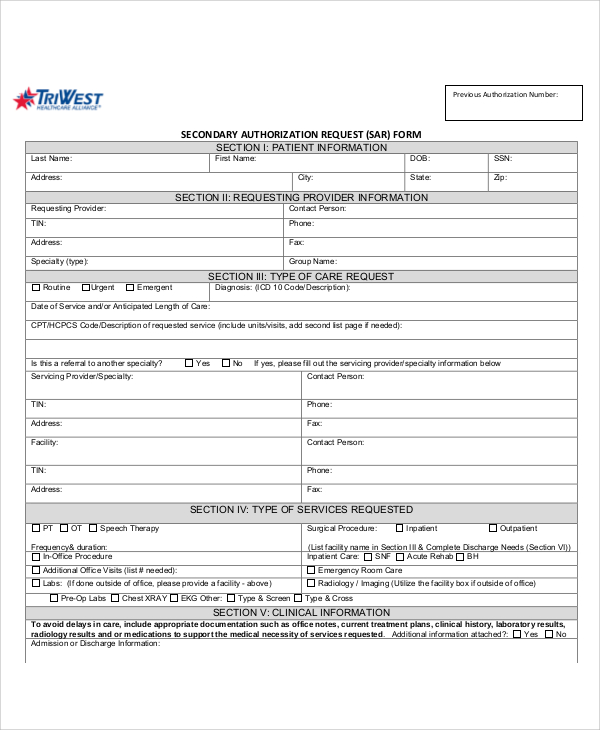
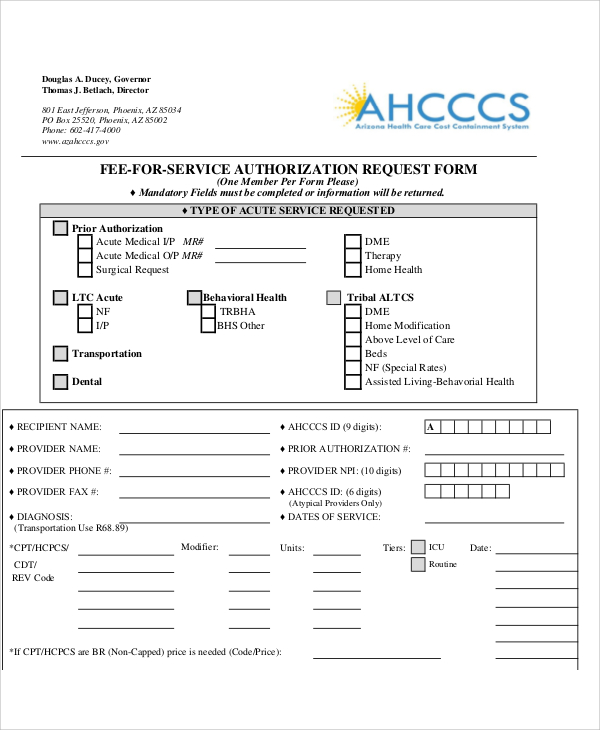
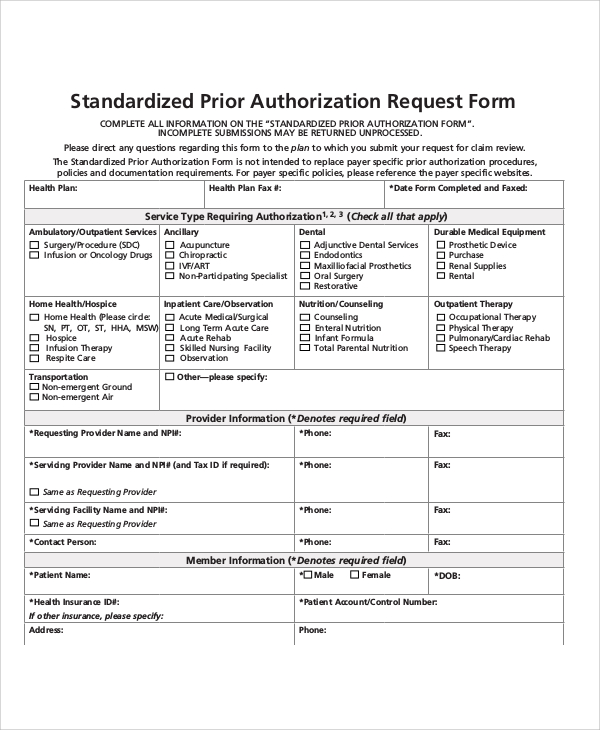
Request For Authorization Form - The form authorizes release of information in accordance with the health insurance portability and accountability act, 45 cfr parts 160 and 164; Web instructions for request for authorization form overview: We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The request for authorization for medical treatment (dwc form rfa) is required for the employee’s treating physician to initiate the utilization review process required by labor code section 4610. A prior authorization form is a requirement used by most insurance companies in the united states for them to determine if a procedure, service, or medication can be covered by terms governing an individual’s insurance portfolio. Web an authorization form is a document that grants permission to an individual or organisation to proceed with certain actions. Web the information requested on this form is solicited under title 38 u.s.c. Web request for authorization of additional classification and rate. Web when your healthcare provider submits a request for prior authorization or appeals a rejected prior authorization, they should: 5701 and 7332 that you specify.
Web request for authorization of additional classification and rate. Request for authorization of additional classification and rate. Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. 5701 and 7332 that you specify. Web instructions for request for authorization form overview: Web when your healthcare provider submits a request for prior authorization or appeals a rejected prior authorization, they should: Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting. The request for authorization for medical treatment (dwc form rfa) is required for the employee’s treating physician to initiate the utilization review process required by labor code section 4610. Far (48 cfr) 53.222 (f) pdf versions of forms use adobe reader ™. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s.
Web an authorization form is a document that grants permission to an individual or organisation to proceed with certain actions. Web the information requested on this form is solicited under title 38 u.s.c. Request for authorization of additional classification and rate. Web instructions for request for authorization form overview: We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. Far (48 cfr) 53.222 (f) pdf versions of forms use adobe reader ™. Here are 9 authorization form templates to use proxy form The request for authorization for medical treatment (dwc form rfa) is required for the employee’s treating physician to initiate the utilization review process required by labor code section 4610. Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting. Web request for authorization of additional classification and rate.
FREE 35+ Sample Authorization Forms in PDF
Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting. The form authorizes release of information in accordance with the health insurance portability and accountability act, 45 cfr parts 160 and 164; Web request for authorization of additional classification and rate. Just like the authorisation letter, this form can serve as.
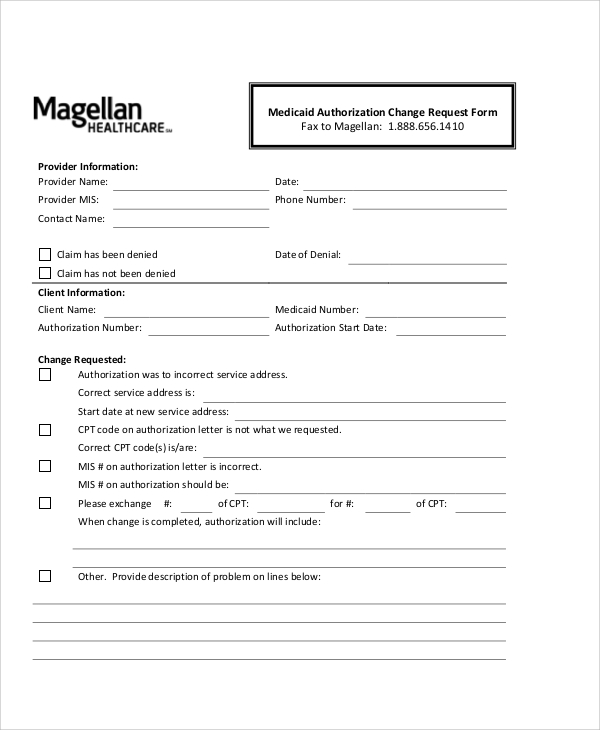
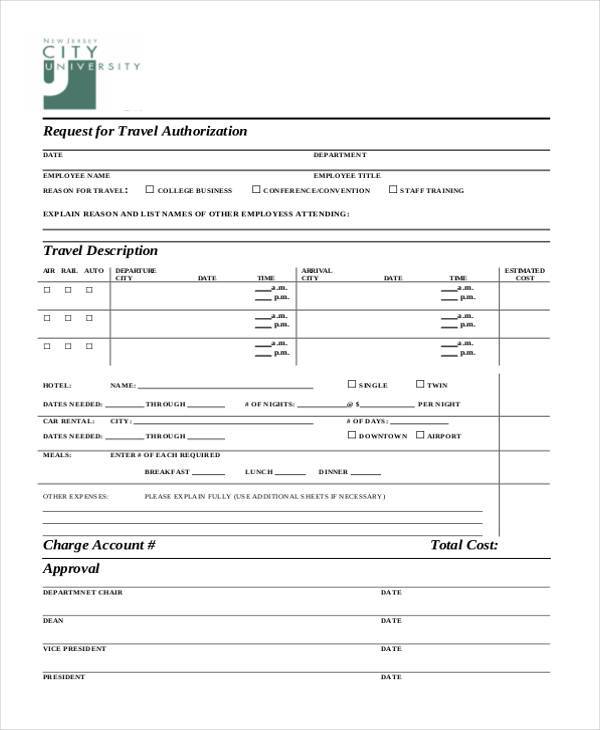
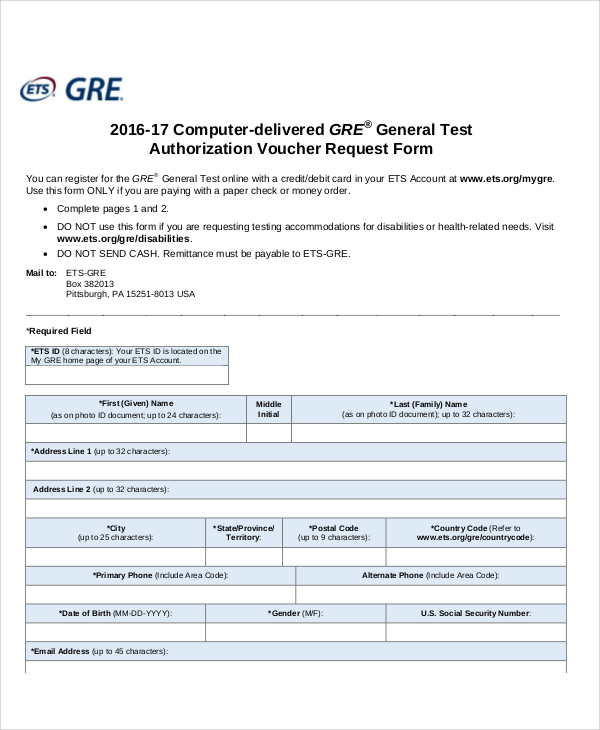
FREE 10+ Sample Authorization Request Forms in MS Word PDF
Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting. Web the information requested on this form is solicited under title 38 u.s.c. Here are 9 authorization form templates.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
Your authorization for power of attorney is recorded on the centralized authorization file (caf) unless line 4, specific use is checked. A prior authorization form is a requirement used by most insurance companies in the united states for them to determine if a procedure, service, or medication can be covered by terms governing an individual’s insurance portfolio. Web request for.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
Your authorization for power of attorney is recorded on the centralized authorization file (caf) unless line 4, specific use is checked. The request for authorization for medical treatment (dwc form rfa) is required for the employee’s treating physician to initiate the utilization review process required by labor code section 4610. 5701 and 7332 that you specify. Web request for authorization.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
Web request for authorization of additional classification and rate. Request for authorization of additional classification and rate. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The form authorizes release of information in accordance with the health insurance portability and accountability act, 45 cfr parts 160 and 164;.
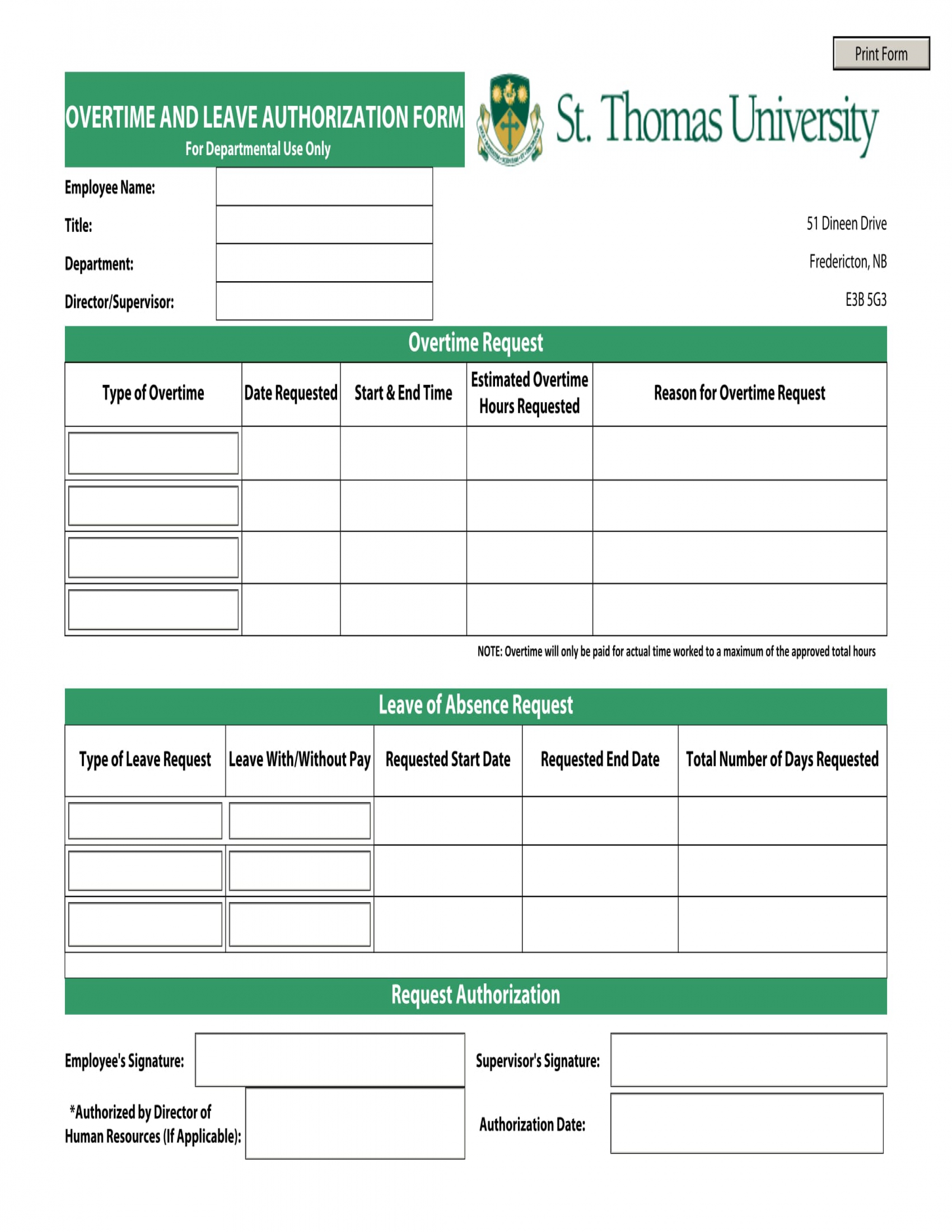
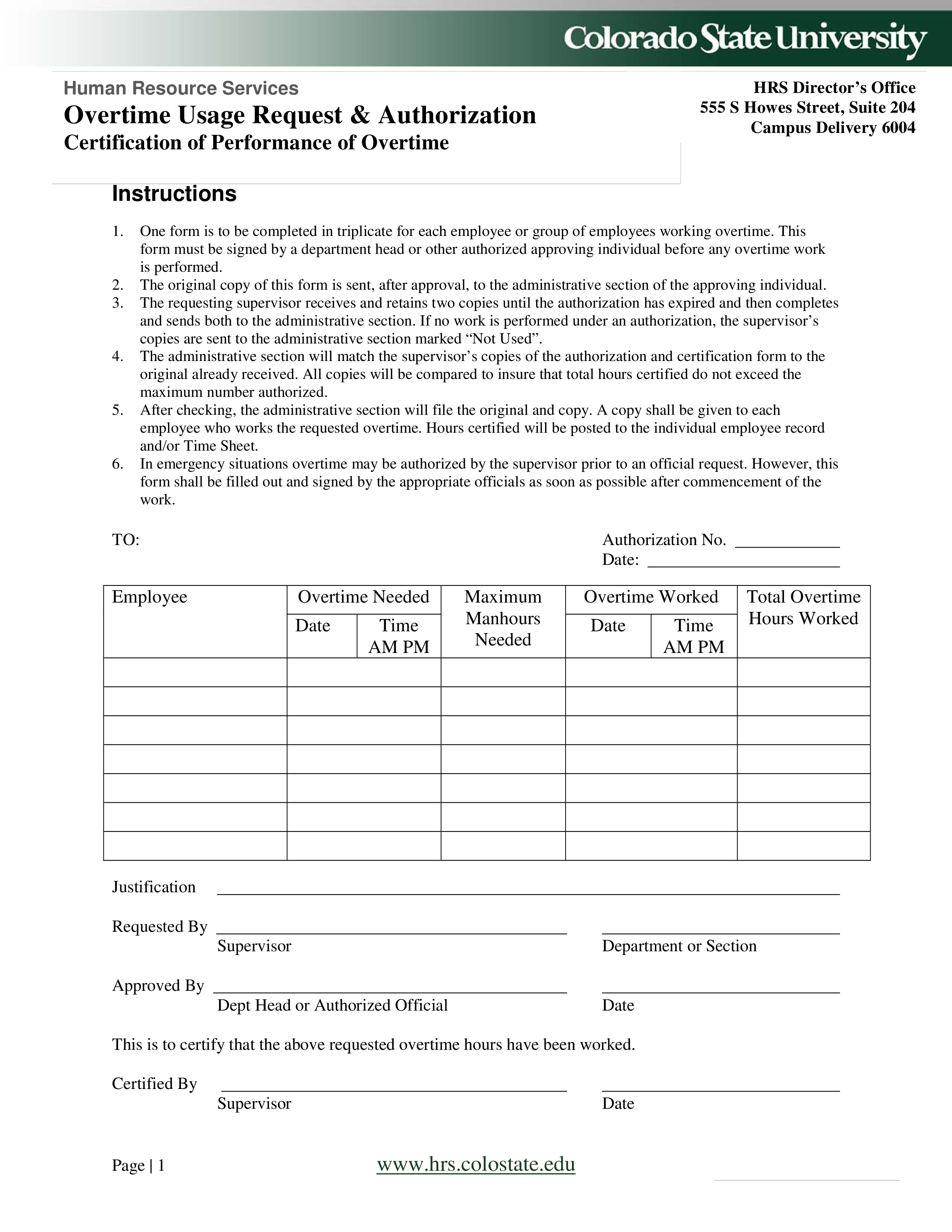
FREE 15+ Overtime Authorization Forms in Excel PDF MS Word
Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. Your authorization for power of attorney is recorded on the centralized authorization file (caf) unless line 4, specific use is checked. Here are 9 authorization form templates to use proxy form A prior authorization form is a requirement.
FREE 41+ Authorization Forms in PDF Excel MS word
Web an authorization form is a document that grants permission to an individual or organisation to proceed with certain actions. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. The form authorizes release of information in accordance with the health insurance portability and accountability act, 45 cfr parts.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
5701 and 7332 that you specify. Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. Web the information requested on this form is solicited under title 38 u.s.c. Here are 9 authorization form templates to use proxy form Web instructions for request for authorization form overview:
FREE 10+ Sample Authorization Request Forms in MS Word PDF
We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. Web request for authorization of additional classification and rate. Web when your healthcare provider submits a request for prior authorization or appeals a rejected prior authorization, they should: Request for authorization of additional classification and rate. The request for.
Overtime Usage Request Authorization Form Templates at
Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. Web the information requested on this form is solicited under title 38 u.s.c. Your authorization for power of attorney is recorded on the centralized authorization file (caf) unless line 4, specific use is checked. Web instructions for request.
Web When Your Healthcare Provider Submits A Request For Prior Authorization Or Appeals A Rejected Prior Authorization, They Should:
Web the information requested on this form is solicited under title 38 u.s.c. Web request for authorization of additional classification and rate. A prior authorization form is a requirement used by most insurance companies in the united states for them to determine if a procedure, service, or medication can be covered by terms governing an individual’s insurance portfolio. Include clinical information that shows the reviewer you’ve met the guidelines for the test, service, or drug you’re requesting.
Web Instructions For Request For Authorization Form Overview:
Web an authorization form is a document that grants permission to an individual or organisation to proceed with certain actions. Your authorization for power of attorney is recorded on the centralized authorization file (caf) unless line 4, specific use is checked. We’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s. 5701 and 7332 that you specify.
Here Are 9 Authorization Form Templates To Use Proxy Form
Just like the authorisation letter, this form can serve as evidence in a court of law in the case of any eventualities. The request for authorization for medical treatment (dwc form rfa) is required for the employee’s treating physician to initiate the utilization review process required by labor code section 4610. Far (48 cfr) 53.222 (f) pdf versions of forms use adobe reader ™. Request for authorization of additional classification and rate.
The Record Lets Irs Assistors Verify Your Permission To Speak With Your.
The form authorizes release of information in accordance with the health insurance portability and accountability act, 45 cfr parts 160 and 164;