Meridian Outpatient Prior Authorization Form
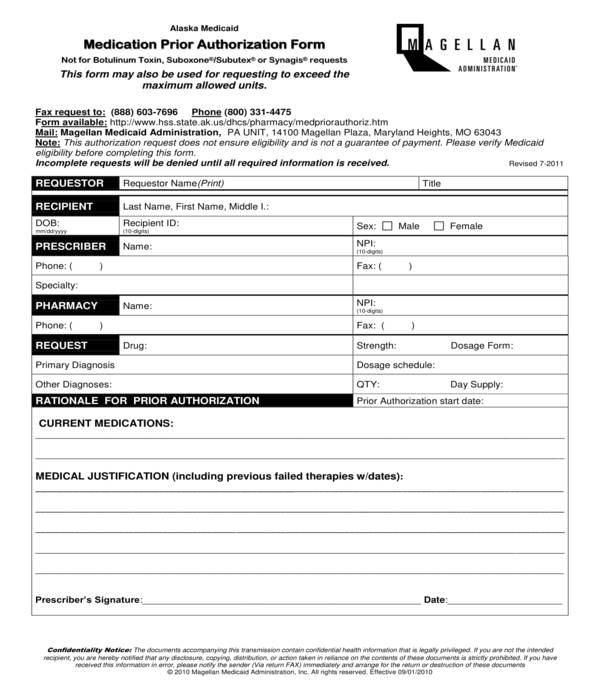
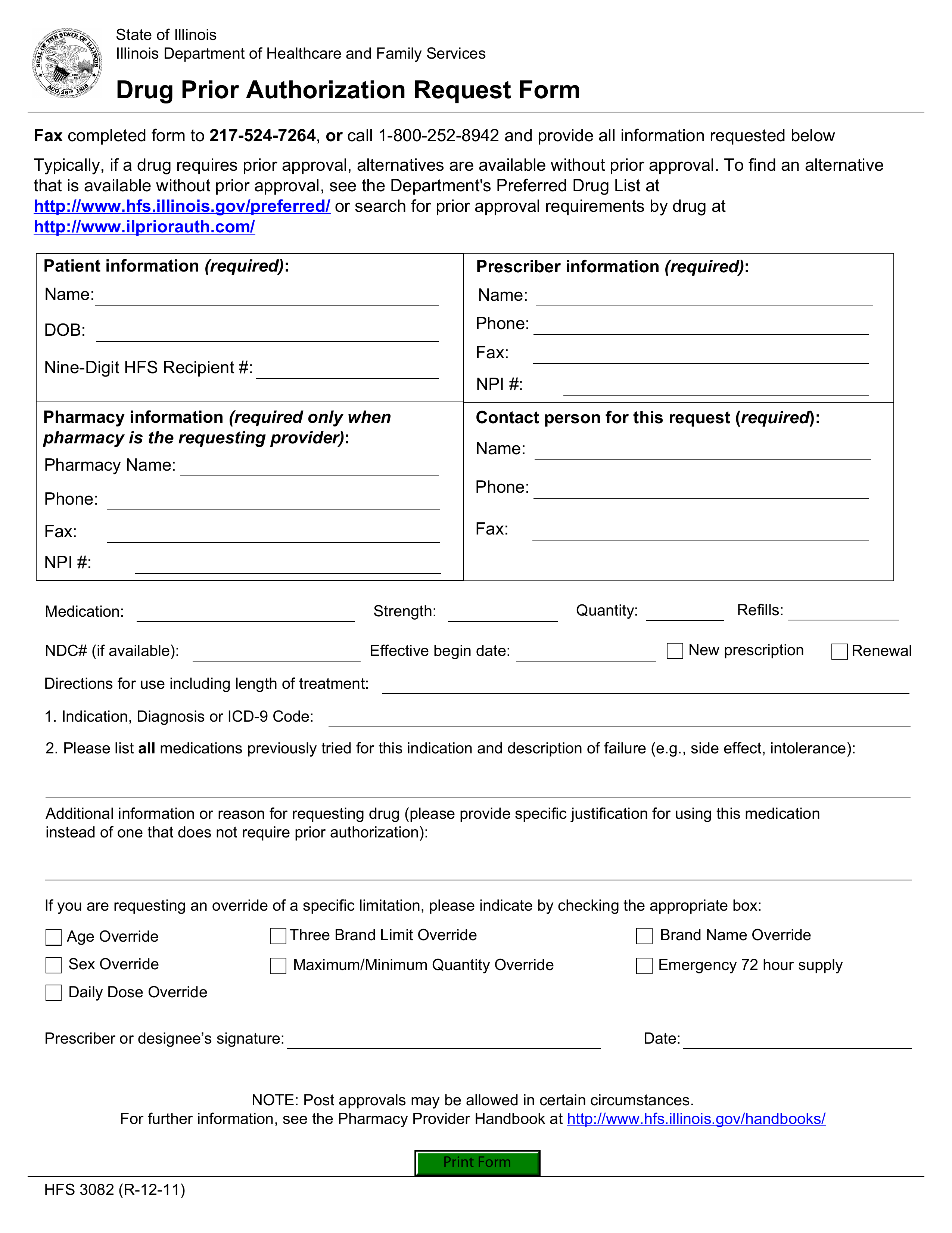
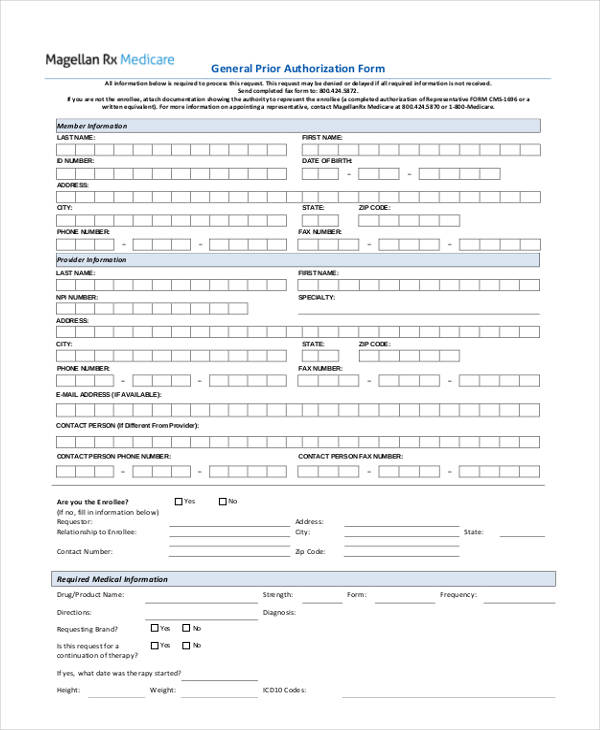
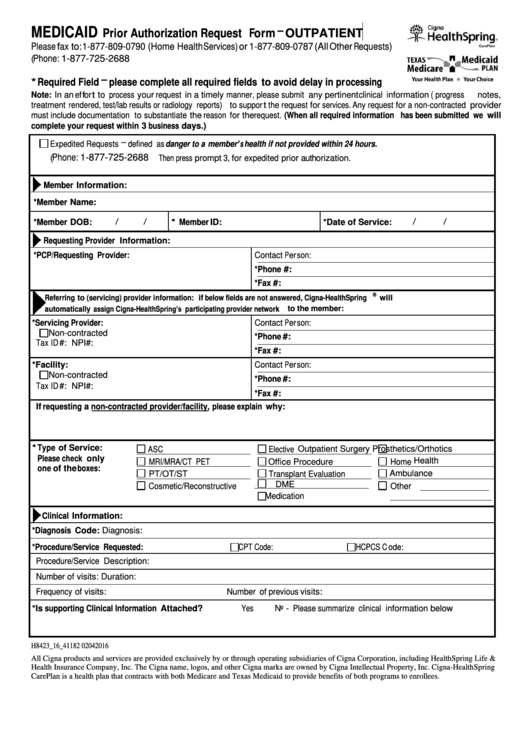
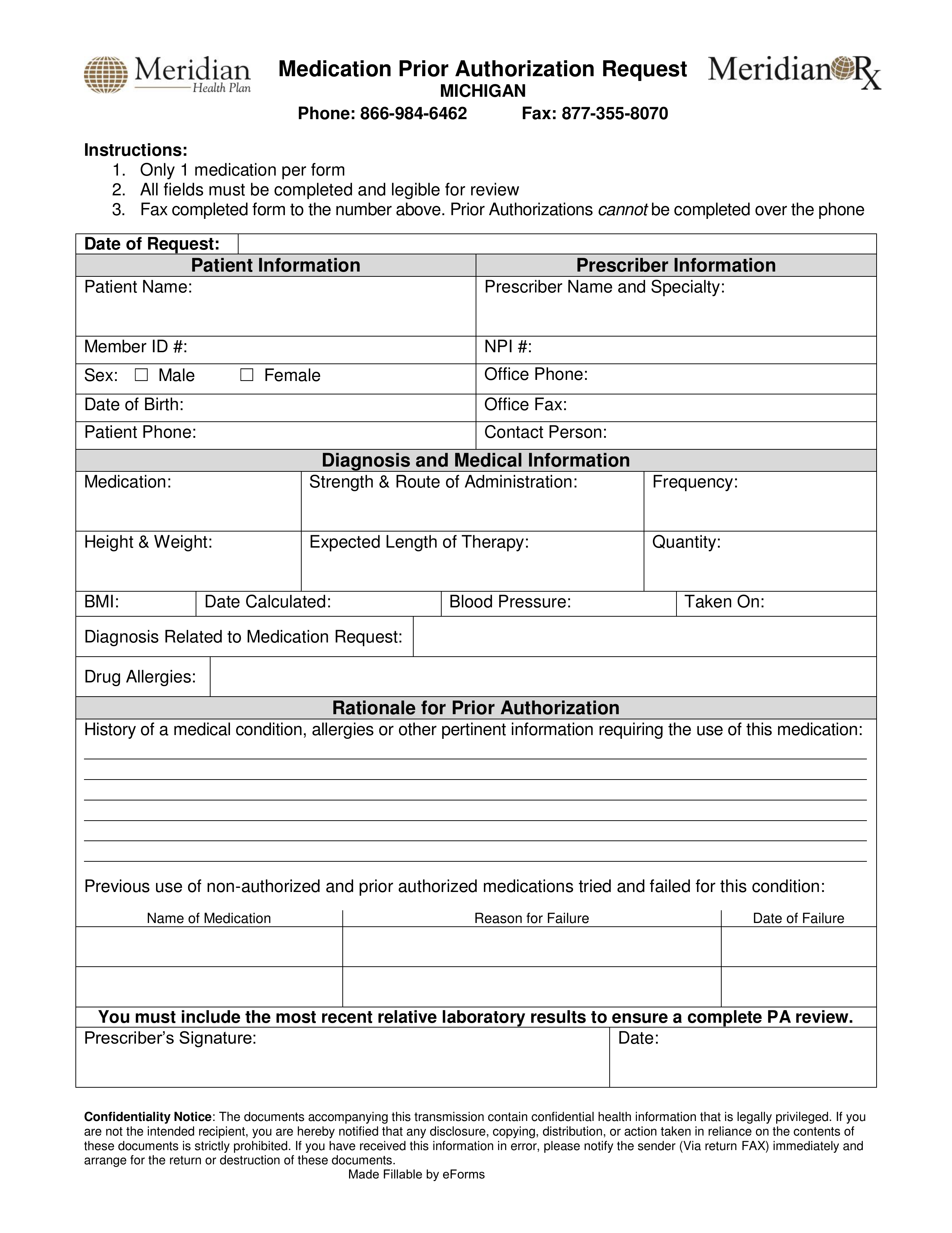
Meridian Outpatient Prior Authorization Form - My health pays rewards® ways to save; Only 1 medication per form all fields must be completed and legible for. Web medication prior authorization request phone: Web outpatient complete and fax to: Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web once you have created an account, you can use the meridian provider portal to: Web biopharmacy outpatient prior authorization fax form (pdf) provider request for reconsideration and claim dispute form (pdf) prior authorization request form for. Online pharmacy prior authorization (pa). Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). The following grid outlines all.
Online pharmacy prior authorization (pa). Only 1 medication per form all fields must be completed and legible for. Web medical referrals & authorizations. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Web outpatient medicaid prior authorization form buy & bill drug requests: Web meridian has created a universal form to improve efficiencies for the authorization process. The following grid outlines all. Web (this will open in a new window). Medication prior authorization request form. Web formulary exception form.
Web once you have created an account, you can use the meridian provider portal to: Meridian partners with several external entities to manage prior authorizations for certain services or populations. Medication prior authorization request form. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web outpatient medicaid prior authorization form buy & bill drug requests: Web (this will open in a new window). Use the meridian tool to see if a pre. Submit the form online on this page. Web home our health plans show our health plans menu about our plans; Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa).
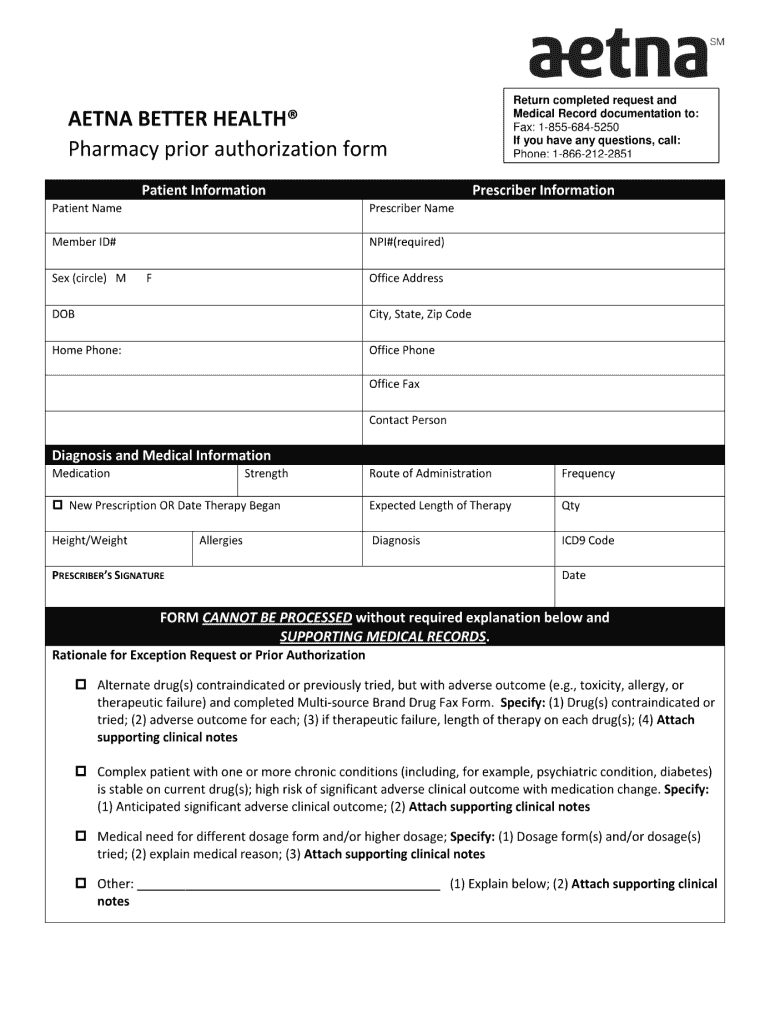
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web meridian has created a universal form to improve efficiencies for the authorization process. Web medication prior authorization request phone: You do not need a paper referral from meridian to see a. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web outpatient complete and fax to:
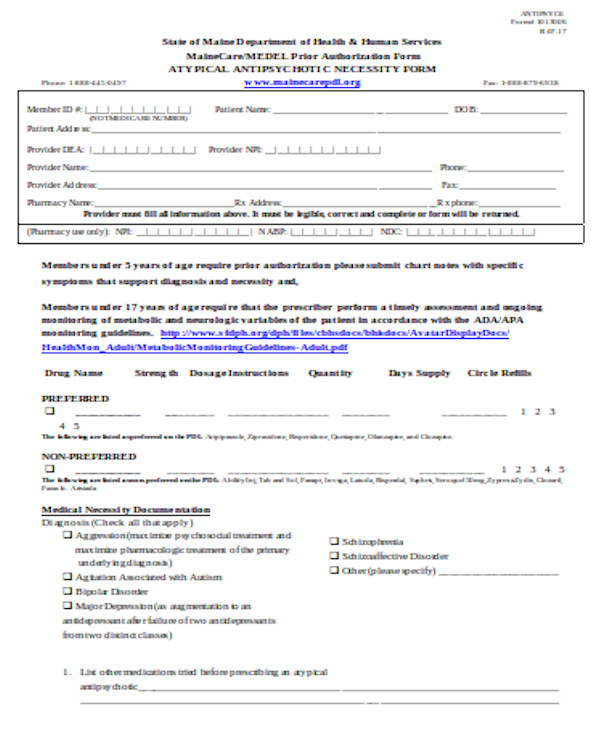
FREE 13+ Prior Authorization Forms in PDF MS Word
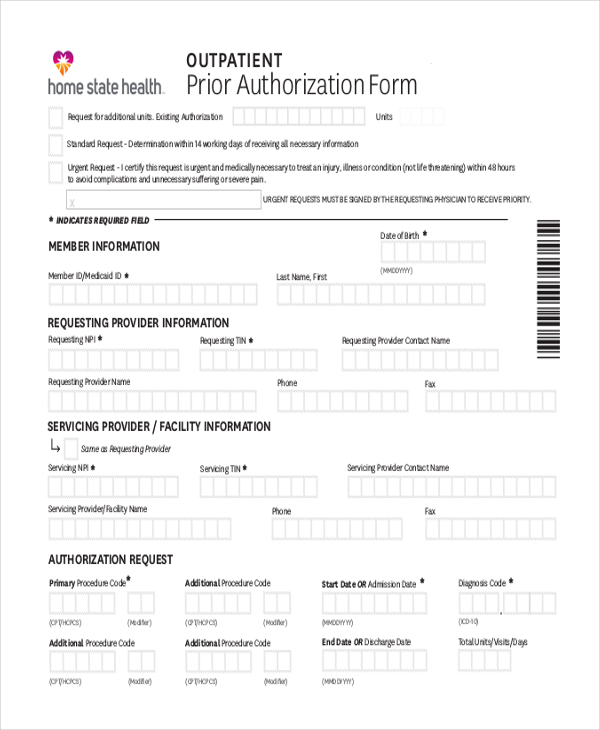
The following grid outlines all. My health pays rewards® ways to save; Web once you have created an account, you can use the meridian provider portal to: Web outpatient medicaid prior authorization form outpatient medicaidprior authorization form request for additional units. Web outpatient complete and fax to:
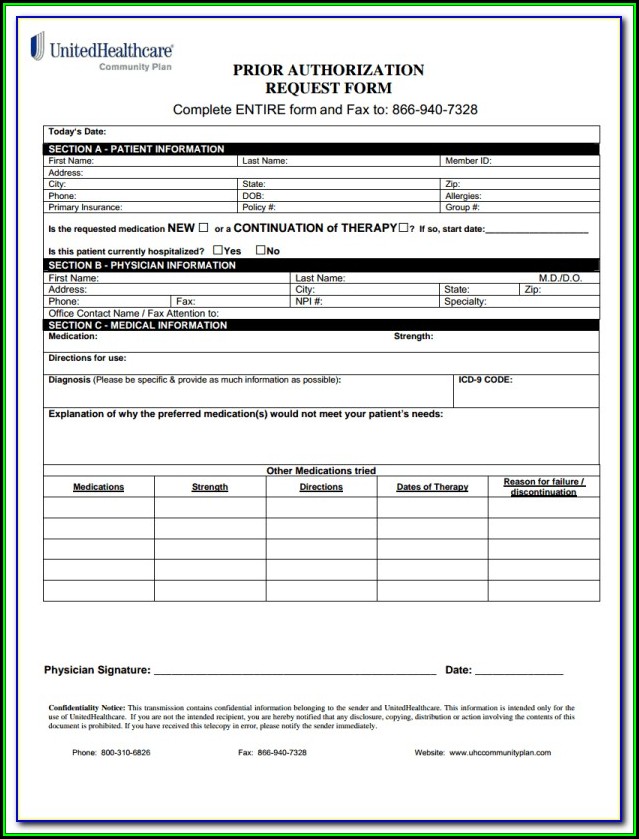
Optumrx Prior Authorization Form Cialis Rx Prior Authorization
Biopharmacy outpatient prior authorization fax form keywords:. Web outpatient medicaid prior authorization form buy & bill drug requests: Web once you have created an account, you can use the meridian provider portal to: Use the meridian tool to see if a pre. Web biopharmacy outpatient prior authorization fax form (pdf) provider request for reconsideration and claim dispute form (pdf) prior.
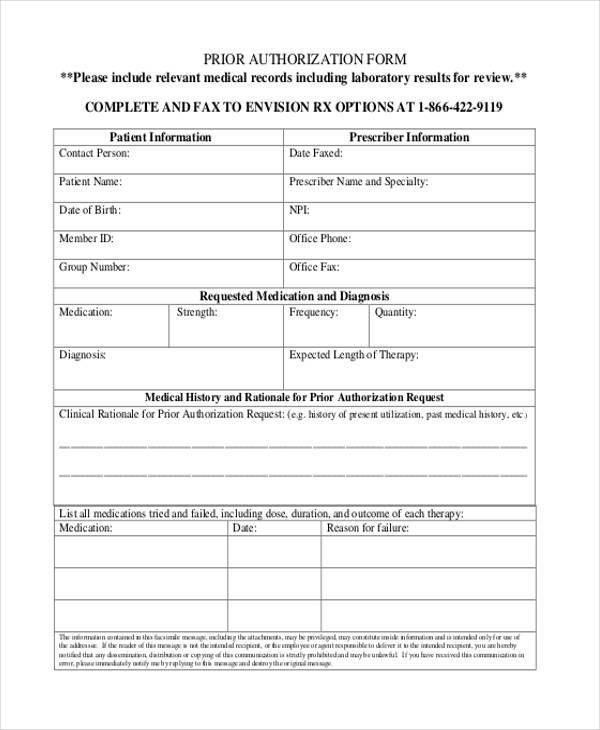
FREE 35+ Sample Authorization Forms in PDF
Medication prior authorization request form. My health pays rewards® ways to save; You do not need a paper referral from meridian to see a. Web biopharmacy outpatient prior authorization fax form (pdf) provider request for reconsideration and claim dispute form (pdf) prior authorization request form for. Web some covered services or medications may need approval from meridian, this is called.
FREE 11+ Prior Authorization Forms in PDF MS Word
Web formulary exception form. Web meridian has created a universal form to improve efficiencies for the authorization process. Online pharmacy prior authorization (pa). Web biopharmacy outpatient prior authorization fax form (pdf) provider request for reconsideration and claim dispute form (pdf) prior authorization request form for. Web prior authorization is required before certain services are rendered to confirm medical necessity as.
Free Illinois Medicaid Prior (Rx) Authorization Form PDF eForms
Web meridian has created a universal form to improve efficiencies for the authorization process. Meridian partners with several external entities to manage prior authorizations for certain services or populations. Web medication prior authorization request phone: Submit the form online on this page. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa).
FREE 13+ Prior Authorization Forms in PDF MS Word
Web home our health plans show our health plans menu about our plans; Web medication prior authorization request phone: Web outpatient complete and fax to: Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web (this will open in a new window).
Fillable Medicaid Prior Authorization Request Form Outpatient Cigna
Web once you have created an account, you can use the meridian provider portal to: My health pays rewards® ways to save; The following grid outlines all. Web meridian has created a universal form to improve efficiencies for the authorization process. Medication prior authorization request form.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Online pharmacy prior authorization (pa). Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Use the meridian tool to see if a pre. Web formulary exception form.
Free Meridian Prior (Rx) Authorization Form PDF eForms
Web medical referrals & authorizations. Web once you have created an account, you can use the meridian provider portal to: Web home our health plans show our health plans menu about our plans; Biopharmacy outpatient prior authorization fax form keywords:. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa).
Web (This Will Open In A New Window).
Web meridian has created a universal form to improve efficiencies for the authorization process. Use the meridian tool to see if a pre. Web biopharmacy outpatient prior authorization fax form (pdf) provider request for reconsideration and claim dispute form (pdf) prior authorization request form for. Web home our health plans show our health plans menu about our plans;
Web Some Covered Services Or Medications May Need Approval From Meridian, This Is Called A Prior Authorization (Pa).
Web formulary exception form. Member request for reimbursement form. Web once you have created an account, you can use the meridian provider portal to: Online pharmacy prior authorization (pa).
Biopharmacy Outpatient Prior Authorization Fax Form Keywords:.
Submit the form online on this page. Meridian partners with several external entities to manage prior authorizations for certain services or populations. Web outpatient medicaid prior authorization form buy & bill drug requests: Only 1 medication per form all fields must be completed and legible for.
Web Outpatient Complete And Fax To:
My health pays rewards® ways to save; Web medical referrals & authorizations. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Medication prior authorization request form.