Ambetter Prior Authorization Form Pdf
Ambetter Prior Authorization Form Pdf - Same as requesting provider servicing. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services. Prior authorization guide (pdf) inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) provider fax back form (pdf) mo marketplace out of network form (pdf) ambetter from home state health oncology pathway solutions faqs (pdf) national imaging associates, inc. Lack of clinical information may result in delayed determination. Join ambetter show join ambetter menu See coverage in your area; Drug information drug name and strength: All required fields must be filled in as incomplete forms will be rejected. Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends or holidays. The information contained in this transmission is confidential and may be protected under the health insurance portability and accountability act of 1996.
Servicing provider / facility information. See coverage in your area; The information contained in this transmission is confidential and may be protected under the health insurance portability and accountability act of 1996. Prior authorization guide (pdf) inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) provider fax back form (pdf) mo marketplace out of network form (pdf) ambetter from home state health oncology pathway solutions faqs (pdf) national imaging associates, inc. Web this process is known as prior authorization. ☐ initial ☐ continuation if continuation, provide therapy start date: Copies of all supporting clinical information are required. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf) psychological and neuropsychological testing checklist (pdf) electroconvulsive therapy (ect) checklist (pdf) ambetter behavioral health. All required fields must be filled in as incomplete forms will be rejected. Member id * last name,.
Use your zip code to find your personal plan. Web this process is known as prior authorization. Web services must be a covered benefit and medically necessary with prior authorization as per ambetter policy and procedures. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services. Web visit covermymeds.com/epa/envolverx to begin using this free service. Same as requesting provider servicing. Member id * last name,. Copies of all supporting clinical information are required. See coverage in your area; Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends or holidays.
FREE 11+ Prior Authorization Forms in PDF MS Word
Member id * last name,. Web visit covermymeds.com/epa/envolverx to begin using this free service. All required fields must be filled in as incomplete forms will be rejected. Servicing provider / facility information. Prior authorization guide (pdf) inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) provider fax back form (pdf) mo marketplace out of network form (pdf).
Gallery of Ambetter Prior Authorization form Beautiful Kircblog 2015
Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends or holidays. Find and enroll in a plan that's right for you. Drug information drug name and strength: Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form.
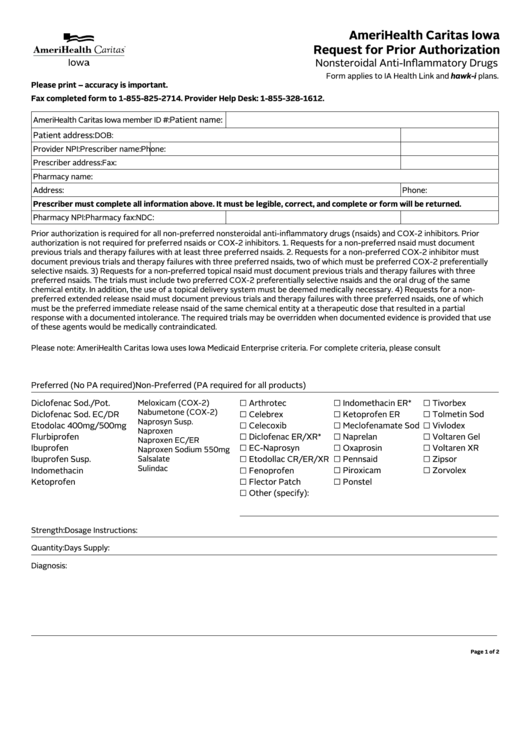
Fillable Request For Prior Authorization Form printable pdf download
Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf) psychological and neuropsychological testing checklist (pdf) electroconvulsive therapy (ect) checklist (pdf) ambetter behavioral health. All required fields must be filled in as incomplete forms will be rejected. Web services must be a covered.
Gallery of Ambetter Prior Authorization form Beautiful Kircblog 2015
Use your zip code to find your personal plan. ☐ initial ☐ continuation if continuation, provide therapy start date: Web this process is known as prior authorization. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services. Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will.
Gallery of Ambetter Prior Authorization form Beautiful Kircblog 2015
All required fields must be filled in as incomplete forms will be rejected. Web services must be a covered benefit and medically necessary with prior authorization as per ambetter policy and procedures. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services. When we receive your prior authorization request, our.
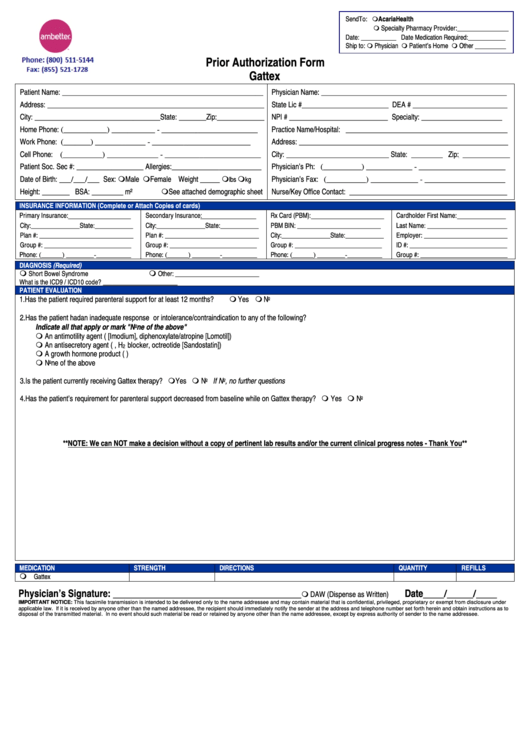
Ambetter Prior Authorization Form Gattex printable pdf download
To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services. Join ambetter show join ambetter menu Web prior authorization fax form fax to: Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf).
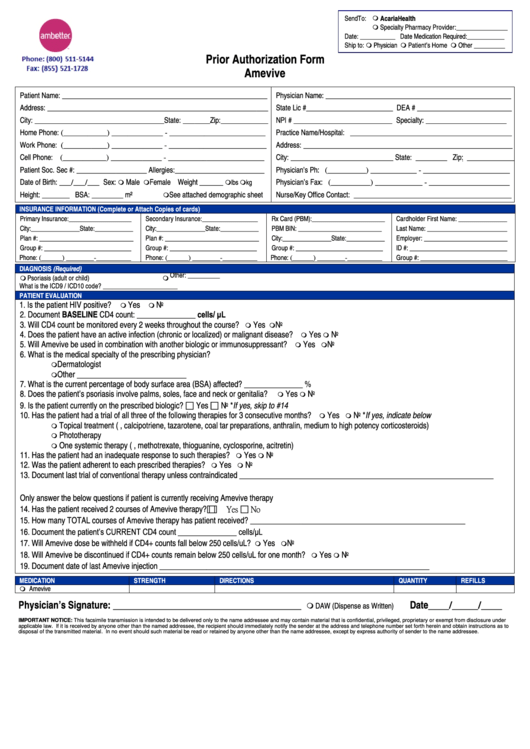
Ambetter Prior Authorization Form Amevive printable pdf download
Lack of clinical information may result in delayed determination. Web services must be a covered benefit and medically necessary with prior authorization as per ambetter policy and procedures. When we receive your prior authorization request, our nurses and doctors will review it. Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will respond via fax or phone.
Medicare Part D Medco Prior Authorization Form Printable
Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf) psychological and neuropsychological testing checklist (pdf) electroconvulsive therapy (ect) checklist (pdf) ambetter behavioral health. Web services must be a covered benefit and medically necessary with prior authorization as per ambetter policy and procedures..
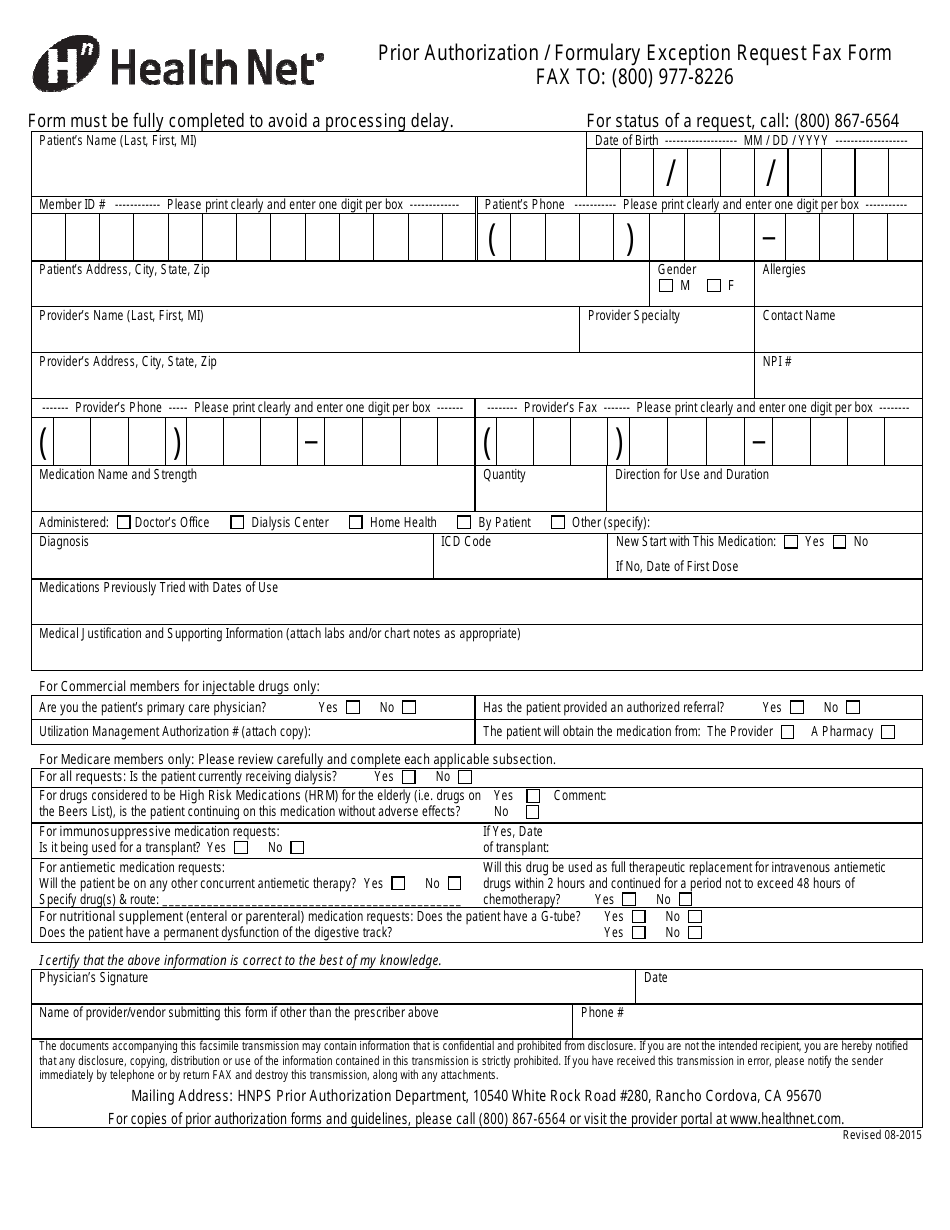
Prior Authorization/Formulary Exception Request Fax Form Health Net
Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf) psychological and neuropsychological testing checklist (pdf) electroconvulsive therapy (ect) checklist (pdf) ambetter behavioral health. When we receive your prior authorization request, our nurses and doctors will review it. See coverage in your area;.
Gallery of Ambetter Prior Authorization form Beautiful Kircblog 2015
Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) change of provider request form (pdf) transcranial magnetic stimulation services prior authorization checklist (pdf) psychological and neuropsychological testing checklist (pdf) electroconvulsive therapy (ect) checklist (pdf) ambetter behavioral health. All required fields must be filled in as incomplete forms will be rejected. Use your zip code to find.
The Information Contained In This Transmission Is Confidential And May Be Protected Under The Health Insurance Portability And Accountability Act Of 1996.
Lack of clinical information may result in delayed determination. Web prior authorization fax form fax to: When we receive your prior authorization request, our nurses and doctors will review it. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or member services.
Servicing Provider / Facility Information.
Or fax this completed form to 866.399.0929 envolve pharmacy solutions and ambetter will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends or holidays. Join ambetter show join ambetter menu Same as requesting provider servicing. ☐ initial ☐ continuation if continuation, provide therapy start date:
Copies Of All Supporting Clinical Information Are Required.
Prior authorization guide (pdf) inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) provider fax back form (pdf) mo marketplace out of network form (pdf) ambetter from home state health oncology pathway solutions faqs (pdf) national imaging associates, inc. See coverage in your area; Find and enroll in a plan that's right for you. Yes no ☐ ☐ ☐ therapy status:
Use Your Zip Code To Find Your Personal Plan.
All required fields must be filled in as incomplete forms will be rejected. Drug information drug name and strength: Member id * last name,. Web services must be a covered benefit and medically necessary with prior authorization as per ambetter policy and procedures.