Ambetter Appeals Form
Ambetter Appeals Form - If you wish to file a grievance or an appeal, please complete this form. Web additionally, information regarding the complaint/grievance and appeal process can be found on our website at ambetter.buckeyehealthplan.com or by calling ambetter at 1. The procedures for filing a. Use your zip code to find your personal plan. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. The completed form or your letter should be mailed to:. Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. An expedited appeal for urgent matters, and a standard appeal. The authorization appeal must be submitted within 180 calendar. If you do not have access to a phone, you can complete this form or write a letter that.
Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. This could be a denial of coverage for requested medical care or for a claim you filed for. Web there are two types of appeals: If you do not have access to a phone, you can complete this form or write a letter that. The procedures for filing a. Web additionally, information regarding the complaint/grievance and appeal process can be found on our website at ambetter.buckeyehealthplan.com or by calling ambetter at 1. Web all ambetter from arizona complete health members are entitled to a complaint/grievance and appeals process if a member is displeased with any aspect of services rendered. Web appeal you file an appeal in response to a denial received from ambetter from health net. All fields are required information a request for reconsideration (level. The appeals operate in a similar.
If you do not have access to a phone, you can complete this form or write a letter that. Learn more at ambetter from sunshine. If you wish to file a grievance or an appeal, please complete this form. The authorization appeal must be submitted within 180 calendar. Disputes of denials for code editing policy. Web there are two types of appeals: Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. Web ambetter claim reconsideration and appeal quick reference guide (pdf) ambetter virtual access referral guide; The procedures for filing a. Web use this form as part of the ambetter of tennessee request for reconsideration and claim dispute process.
Envolve Vision Newsletter Volume 6 Issue 3 National English
Web authorization and coverage complaints must follow the appeal process below. Use your zip code to find your personal plan. Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. The authorization appeal must be submitted within 180 calendar. This could be a denial of coverage for requested medical care or.
Who Accepts Ambetter Health Insurance insurance
Web there are two types of appeals: Ambetter virtual access training (pdf). This could be a denial of coverage for requested medical care or for a claim you filed for. The procedures for filing a. The completed form or your letter should be mailed to:.
Ambetter Health Insurance Ambetter Reviews and Complaints 2020
Web all ambetter from arizona complete health members are entitled to a complaint/grievance and appeals process if a member is displeased with any aspect of services rendered. If you choose not to complete this form, you may write a letter that includes the information requested below. Web additionally, information regarding the complaint/grievance and appeal process can be found on our.
Ambetter Health Insurance Coverage For Drug Rehab
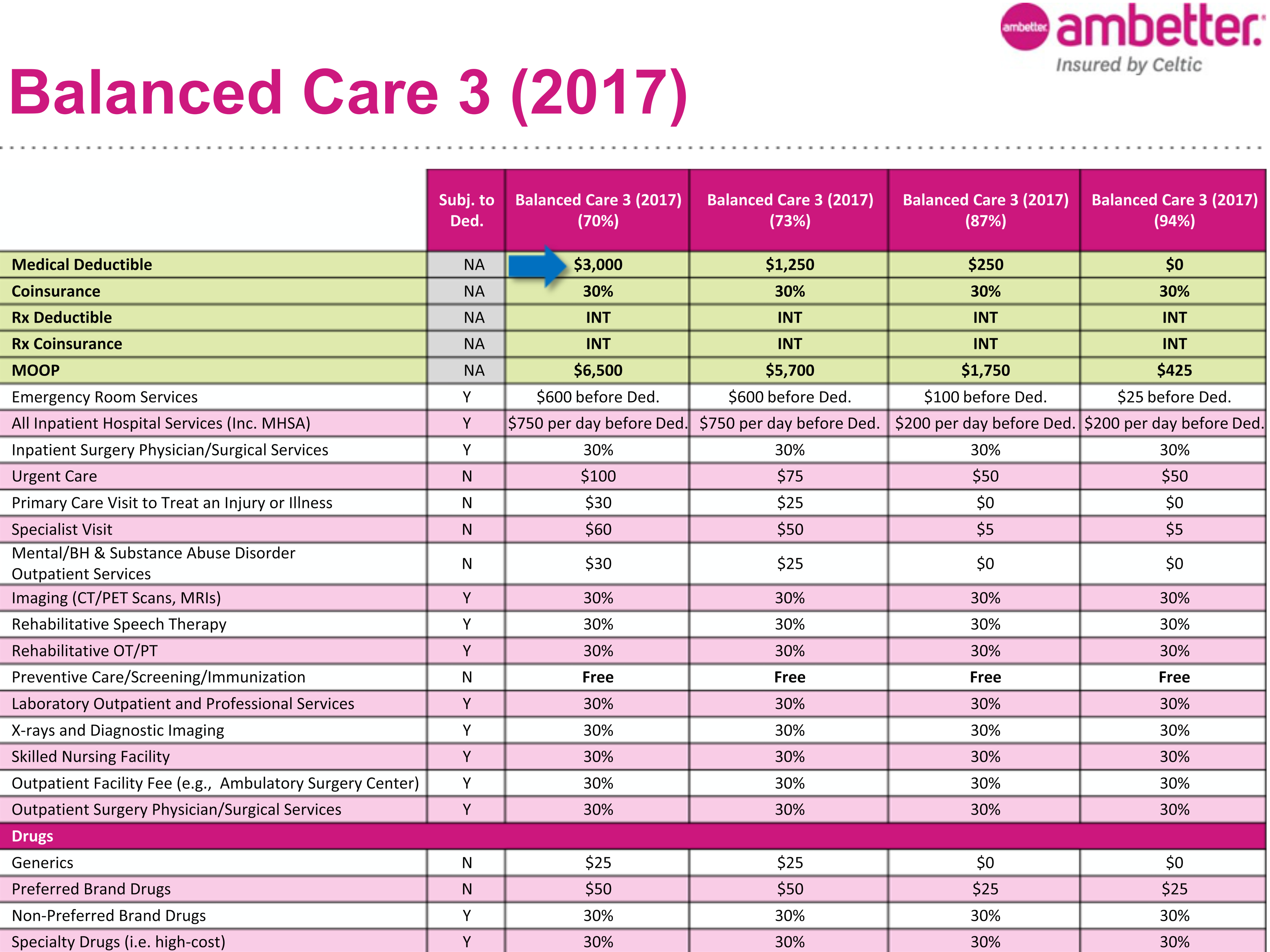
Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Learn more at ambetter from sunshine. Web inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) grievance and appeals; The completed form or your letter should be mailed to:. If you do not have access to a.
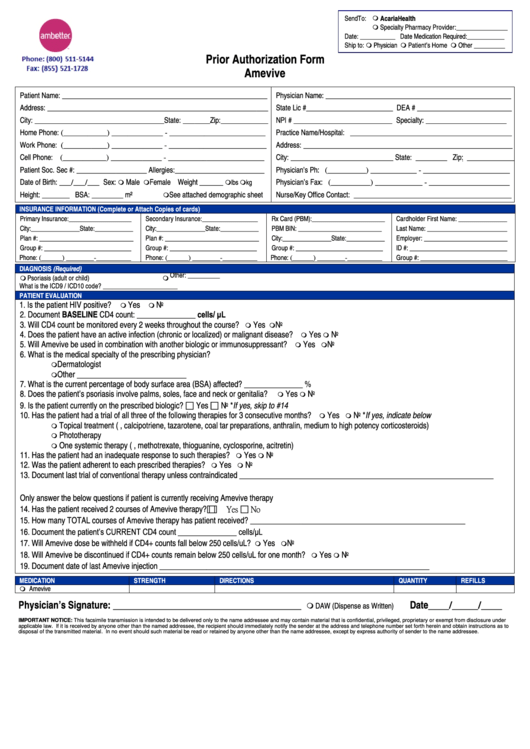
Ambetter Prior Authorization Form Amevive printable pdf download
Web ambetter claim reconsideration and appeal quick reference guide (pdf) ambetter virtual access referral guide; Web authorization and coverage complaints must follow the appeal process below. Ambetter virtual access training (pdf). Web grievance or appeal form. The procedures for filing a.
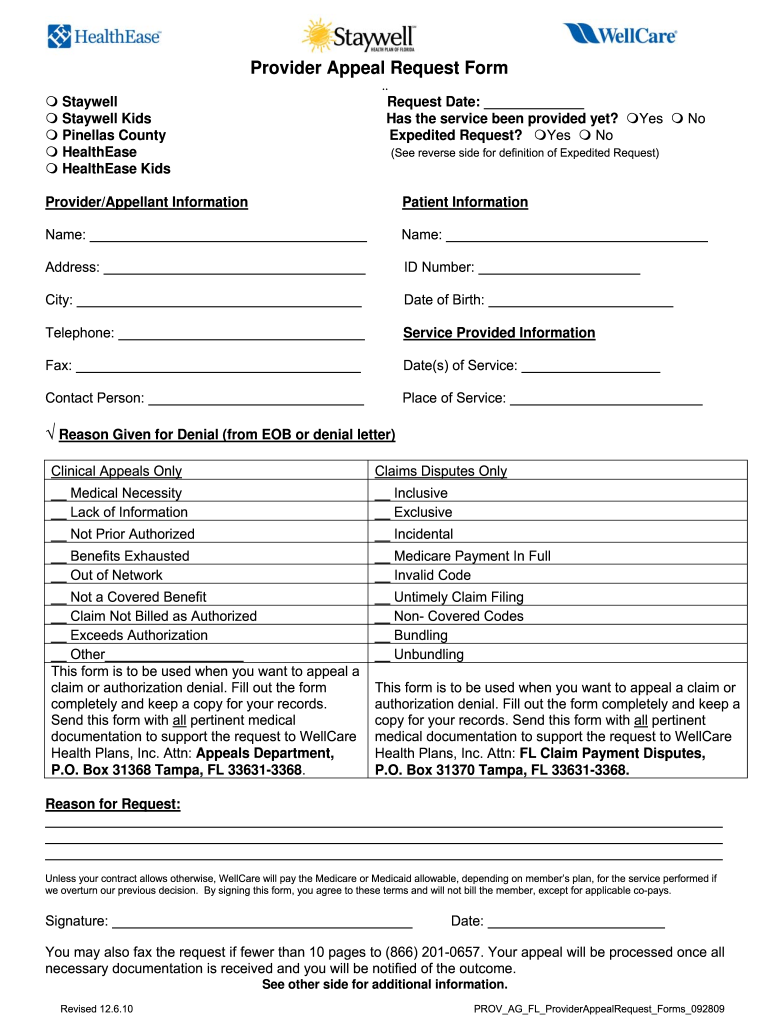
Wellcare Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
Web ambetter claim reconsideration and appeal quick reference guide (pdf) ambetter virtual access referral guide; Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. See coverage in your area; If you choose not to complete this form,. Learn more at ambetter from sunshine.
Who Accepts Ambetter Health Insurance insurance
If you choose not to complete this form,. Web appeal you file an appeal in response to a denial received from ambetter from health net. Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. Web use this form as part of the ambetter of tennessee request for reconsideration and claim.
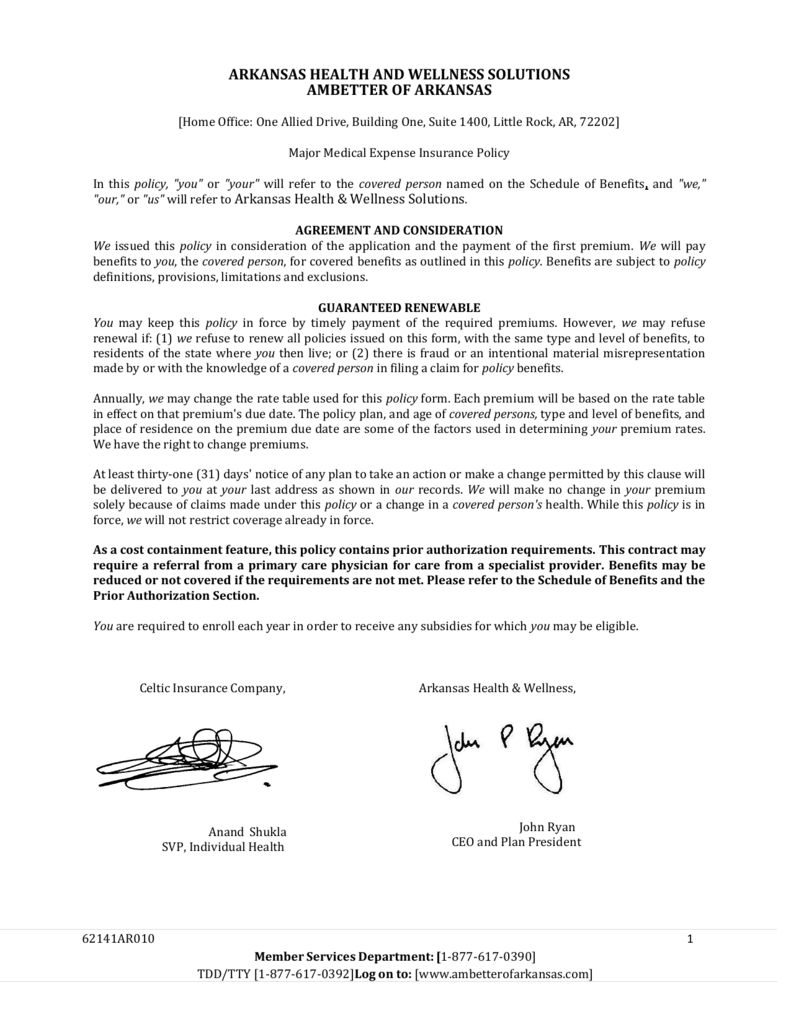
Ambetter of Arkansas Major Medical Expense Insurance Policy
If you wish to file a grievance or an appeal, please complete this form. Use your zip code to find your personal plan. Each type of appeal has three levels available. Web all ambetter from arizona complete health members are entitled to a complaint/grievance and appeals process if a member is displeased with any aspect of services rendered. Web to.
Ambetter Insurance Review What You Need to Know Editorialge
An appeal is the mechanism which allows providers the right to appeal actions of ambetter such as a. If you wish to file a grievance or an appeal, please complete this form. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. Learn more at ambetter from sunshine. Web additionally, information regarding.
Ambetter Insurance Review My Experience MoneyUnder30
Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. If you wish to file a grievance or an appeal, please complete this form. Ambetter virtual access training (pdf). Learn more at ambetter from sunshine. See coverage in your area;
An Expedited Appeal For Urgent Matters, And A Standard Appeal.
Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Each type of appeal has three levels available. Web use this form as part of the ambetter of tennessee request for reconsideration and claim dispute process. Web authorization and coverage complaints must follow the appeal process below.
If You Wish To File A Grievance Or An Appeal, Please Complete This Form.
Web grievance or appeal form. Web access our member resources from our member handbook, reference materials like a doctor visit checklist, and authorization forms. Web all ambetter from arizona complete health members are entitled to a complaint/grievance and appeals process if a member is displeased with any aspect of services rendered. The appeals operate in a similar.
Disputes Of Denials For Code Editing Policy.
All fields are required information a request for reconsideration (level. This could be a denial of coverage for requested medical care or for a claim you filed for. Durable medical equipment (dme) form (pdf) breast. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review.
See Coverage In Your Area;
Ambetter virtual access training (pdf). Web ambetter claim reconsideration and appeal quick reference guide (pdf) ambetter virtual access referral guide; Web additionally, information regarding the complaint/grievance and appeal process can be found on our website at ambetter.buckeyehealthplan.com or by calling ambetter at 1. If you choose not to complete this form, you may write a letter that includes the information requested below.