Ambetter Appeal Form Florida
Ambetter Appeal Form Florida - Web use this form as part of the ambetter from absolute total care request for reconsideration and claim dispute process. See coverage in your area; With ambetter, you can rely on the services and support that you need to deliver the best quality of. A copy of the eop/eob(s) with claim(s) to be reviewed clearly circled. Web with this claims adjustment request form include: Use your zip code to find your personal plan. Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter member’s evidence of coverage. If you wish to file an appeal in writing,. Web an appeal is a request to review a denied service or referral. All fields are required information a request for.
Web appeal you file an appeal in response to a denial received from ambetter from health net. Web endobj xref 294 156 0000000016 00000 n 0000004342 00000 n 0000004579 00000 n 0000004623 00000 n 0000005338 00000 n 0000005379 00000 n 0000005430 00000 n. If you wish to file an appeal in writing,. Payspan (pdf) secure portal (pdf) provider resource guide (pdf) outpatient. Web use this form as part of the ambetter from absolute total care request for reconsideration and claim dispute process. Web home shop our plans for providers healthy partnerships are our specialty. With ambetter, you can rely on the services and support that you need to deliver the best quality of. Disputes of denials for code editing policy. Get your flu shot preventive services guide (pdf). See coverage in your area;
Disputes of denials for code editing policy. Web appeal you file an appeal in response to a denial received from ambetter from health net. Web use this form as part of the ambetter from coordinated care request for reconsideration and claim dispute process. See coverage in your area; Web use this form as part of the ambetter from absolute total care request for reconsideration and claim dispute process. Use your zip code to find your personal plan. You must file within 90 days of the dispute resolution or when you became aware of the issue. Contact us for more information. For ensure that ambetter member’s rights be protected, all ambetter members are titling at a complaint/grievance and. Web member complaint/grievance and appeal process.
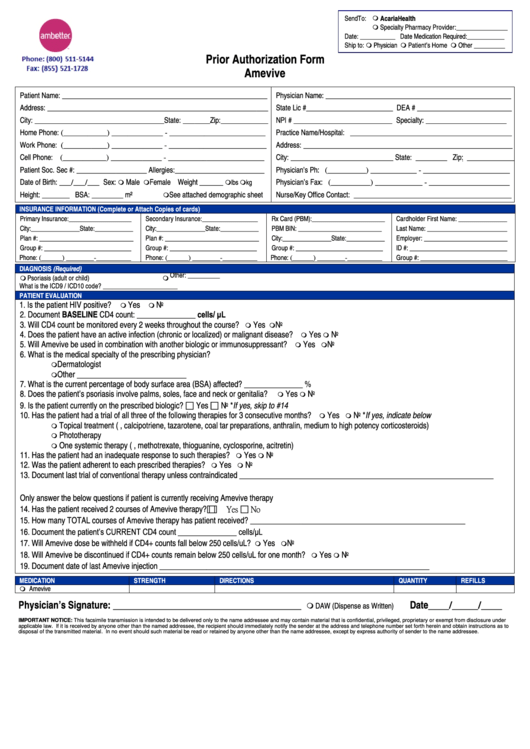
What Is The Group Id For Ambetter / Ambetter Prior Authorization Form
Web member complaint/grievance and appeal process. Web select your state to visit the ambetter site for your coverage area. This could be a denial of coverage for requested medical care or for a claim you filed for. Web appeal you file an appeal in response to a denial received from ambetter from health net. A copy of the eop/eob(s) with.
Ambetter o Florida Blue Obamacare Trumpcare Seguros privados
You can appeal our decision if a service was denied, reduced, or ended early. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. Web ambetter (arizona, florida, georgia, illinois, indiana, kansas, michigan, mississippi, missouri, nevada, new mexico, north carolina, ohio, pennsylvania, south carolina,. Web with this claims adjustment request form include:.
Envolve Vision Newsletter Volume 6 Issue 3 National English
Web an appeal is a request to review a denied service or referral. All fields are required information a request for. Web provider complaint process a complaint is a written expression by a provider which indicates dissatisfaction or dispute with ambetter's policies, procedure, or any aspect of. A request for reconsideration (level i) is. Contact us for more information.
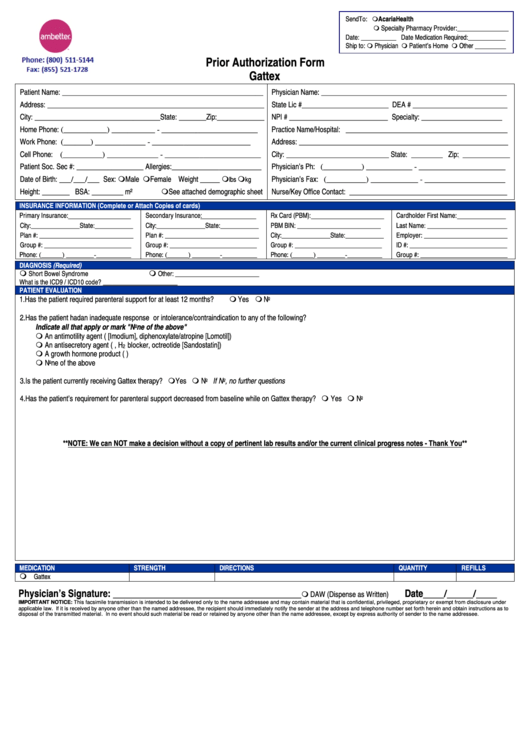
Ambetter Prior Authorization Form Gattex printable pdf download
All fields are required information a request for. The procedures for filing a. Use your zip code to find your personal plan. Web ambetter (arizona, florida, georgia, illinois, indiana, kansas, michigan, mississippi, missouri, nevada, new mexico, north carolina, ohio, pennsylvania, south carolina,. You must file within 90 days of the dispute resolution or when you became aware of the issue.
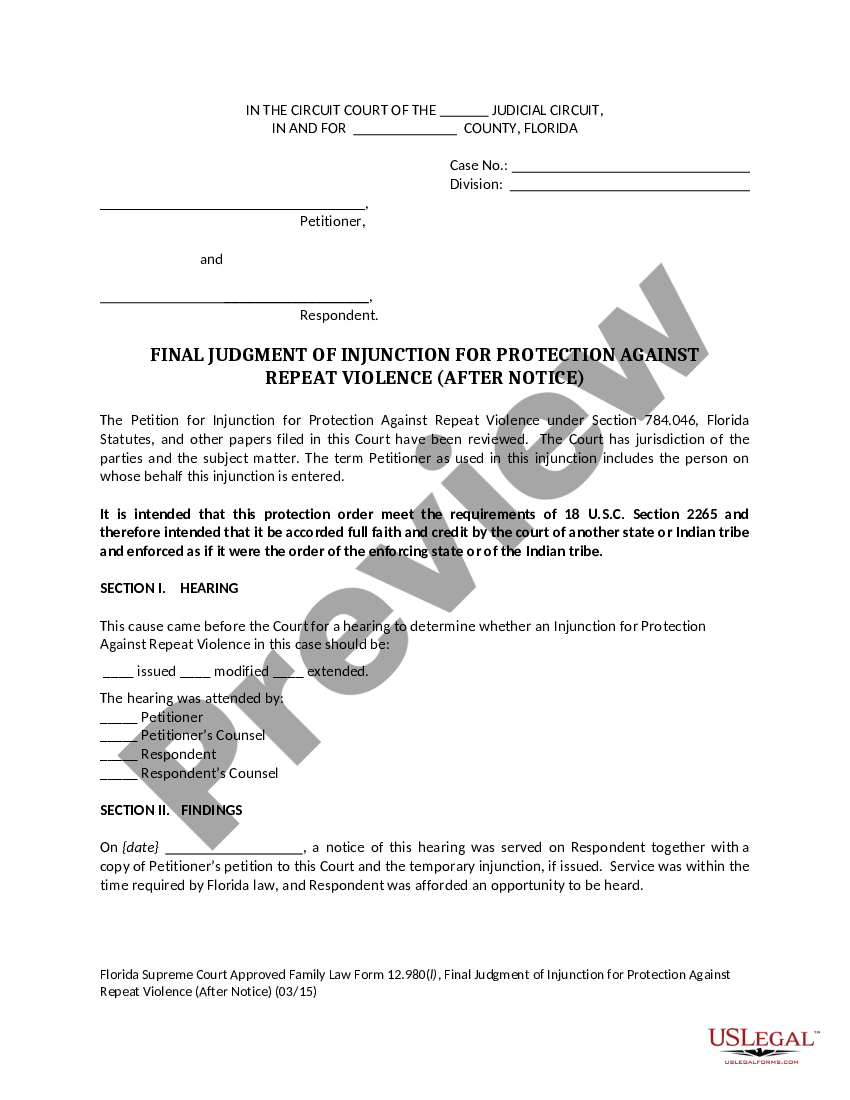
Florida Final Judgment of Injunction for Protection Against Repeat
Web endobj xref 294 156 0000000016 00000 n 0000004342 00000 n 0000004579 00000 n 0000004623 00000 n 0000005338 00000 n 0000005379 00000 n 0000005430 00000 n. See coverage in your area; Web to ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Payspan (pdf) secure portal (pdf) provider resource guide (pdf).
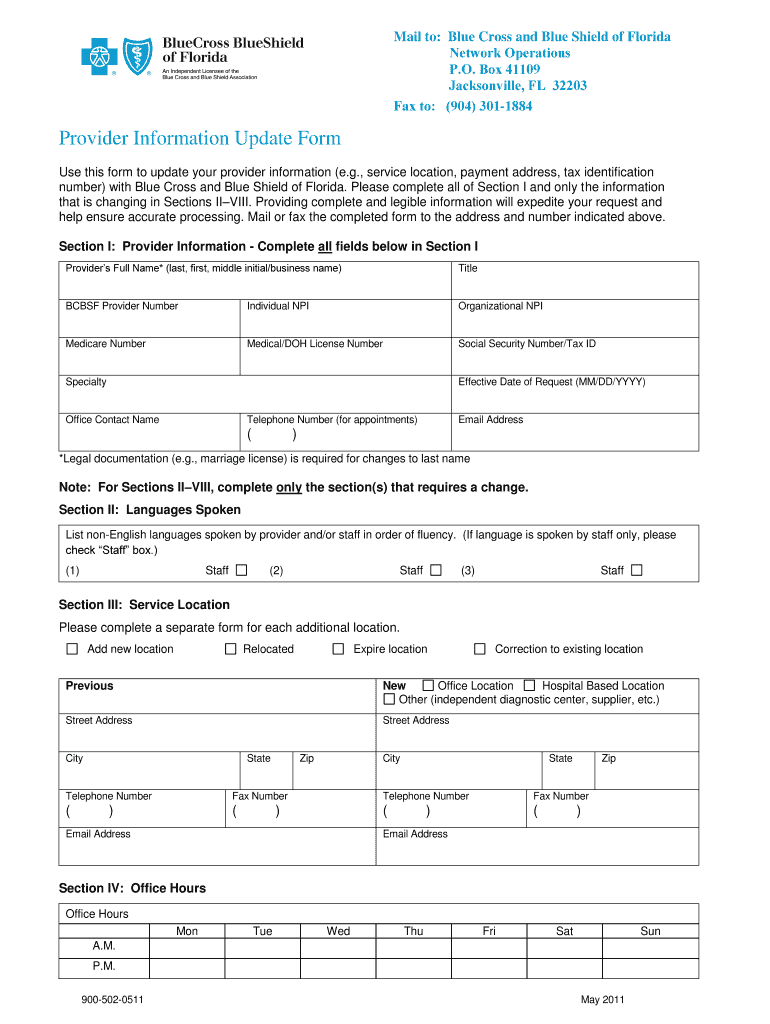
Florida Forms
The procedures for filing a. With ambetter, you can rely on the services and support that you need to deliver the best quality of. Web select your state to visit the ambetter site for your coverage area. Disputes of denials for code editing policy. A copy of the eop/eob(s) with claim(s) to be reviewed clearly circled.
Nics Voluntary Appeal Form eversilicon
Contact us for more information. Use your zip code to find your personal plan. For ensure that ambetter member’s rights be protected, all ambetter members are titling at a complaint/grievance and. See coverage in your area; Web to ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process.
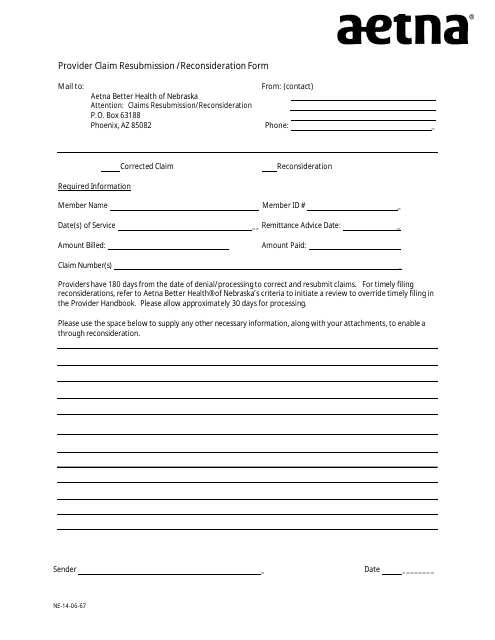
Nebraska Provider Claim Resubmission/Reconsideration Form Aetna
The procedures for filing a. You can appeal our decision if a service was denied, reduced, or ended early. The form may be submitted via:. A copy of the eop/eob(s) with claim(s) to be reviewed clearly circled. Web provider complaint process a complaint is a written expression by a provider which indicates dissatisfaction or dispute with ambetter's policies, procedure, or.
Ambetter Agent Resources Plans And Client Brochures
Web select your state to visit the ambetter site for your coverage area. Web home shop our plans for providers healthy partnerships are our specialty. All fields are required information a request for. The procedures for filing a. A request for reconsideration (level i) is.
Appellants Initial Brief to Florida's 1st District Court of Appeal
See coverage in your area; You can appeal our decision if a service was denied, reduced, or ended early. Web provider complaint process a complaint is a written expression by a provider which indicates dissatisfaction or dispute with ambetter's policies, procedure, or any aspect of. Web use this form as part of the ambetter from coordinated care request for reconsideration.
Web Ambetter (Arizona, Florida, Georgia, Illinois, Indiana, Kansas, Michigan, Mississippi, Missouri, Nevada, New Mexico, North Carolina, Ohio, Pennsylvania, South Carolina,.
Web with this claims adjustment request form include: You can appeal our decision if a service was denied, reduced, or ended early. Web use this form as part of the ambetter from absolute total care request for reconsideration and claim dispute process. See coverage in your area;
You Must File Within 90 Days Of The Dispute Resolution Or When You Became Aware Of The Issue.
The procedures for filing a. The form may be submitted via:. Web appeal you file an appeal in response to a denial received from ambetter from health net. Web select your state to visit the ambetter site for your coverage area.
For Ensure That Ambetter Member’s Rights Be Protected, All Ambetter Members Are Titling At A Complaint/Grievance And.
This could be a denial of coverage for requested medical care or for a claim you filed for. A request for reconsideration (level i) is. Web endobj xref 294 156 0000000016 00000 n 0000004342 00000 n 0000004579 00000 n 0000004623 00000 n 0000005338 00000 n 0000005379 00000 n 0000005430 00000 n. A copy of the eop/eob(s) with claim(s) to be reviewed clearly circled.
Web Member Complaint/Grievance And Appeal Process.
Web to ensure that ambetter member’s rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Web use this form as part of the ambetter from coordinated care request for reconsideration and claim dispute process. If you wish to file an appeal in writing,. Web the procedures for filing a complaint/grievance or appeal are outlined in the ambetter member’s evidence of coverage.